3D Bioengineered Brains – a New Approach to Personalized Cancer Therapy
Learn how tissue bioengineer Dr. Tang-Schomer is working to make personalized medicine a reality for brain cancer patients
10 Mar 2017
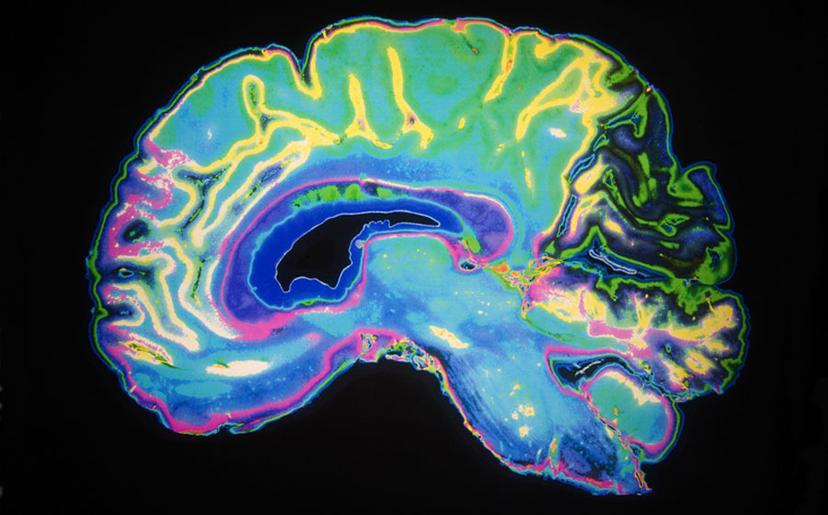
Source: 123rf.com 2014
Dr. Min Tang-Schomer Assistant Professor at Connecticut Children’s Medical Center. Dr. Tang-Schomer is a tissue engineer whose research has a central theme of applying innovative engineering approaches to understand the brain.
Dr. Min Tang-Schomer, Assistant Professor at Connecticut Children’s Medical Center and University of Connecticut Health Center, told SelectScience® about the new direction she is taking with the 3D bioengineered brain-like tissue model she created back in 2014. After starting her career in tissue engineering, Dr. Tang-Schomer’s interest in the brain and neurology encouraged her to move into the field of neuroscience; an area in which she felt bioengineering was being underutilized.
At Tufts University in 2014, as a postdoc., Dr. Tang-Schomer led a team in Dr. David Kaplan's laboratory that developed brain-like cortical tissue using a silk-protein based scaffold, an extracellular matrix composite, and rat primary cortical neurons. The silk-protein scaffold was used to create modules that mimicked grey and white brain matter, which then fitted together like a jigsaw to create a self-supporting structure. The resulting tissue also had good electrophysiological function, allowing it to respond in a way that mimicked cortical tissue in vivo.
“The scaffold means you can use a more engineering approach to creating models. For example, you can add a perfusion system so you can introduce a vascular system into the brain tissue, or you can have more control monitoring the tissue model,” Dr. Tang-Schomer explained.
Since being published in PNAS in 2014, this model has been used and adapted by multiple research groups investigating autism, Parkinson’s disease and microencephaly. However, Dr. Tang-Schomer has taken the research in another direction – personalized cancer treatment.
Personalized brain tumor model
In her current research project, Dr. Tang-Schomer is changing the cell source. Instead of creating the bioengineered tissue from rat neurons or neural stem cells like others using the model, she is using patient brain tumor cells obtained from tumor dissections. The resulting 3D brain tumor models can then be used in pediatric neuro-oncology studies as well as mechanistic drug studies.
“This approach has a lot of advantages. You can create hundreds of clones of the tumor and then use these to test for a wide range of drugs,” she explained. But how do you go about creating an accurate model of a patient’s brain tumor? “Tumors are made up of a heterogeneous cell population and to create an accurate model, you need to know what types of cells there are and what percentage of the population they make up.”
Validating the model using antibody approaches
I’m searching the market to find antibodies which match up to validated clinical antibodies.
Dr. Tang-Schomer described how she used antibodies to profile the cell populations that developed over the culture period in her in vitro model and compared this to the cell populations in the original patient tumor. Assessing this allows her to optimize the cell culture conditions to create models which match the original tumor as closely as possible. Her research relies heavily on flow cytometry for these assessments, as it gives quantitative information about the cell distribution. She also utilizes conventional immunohistochemistry for assessing the success of the model, as when combined with confocal microscopy it gives good 3D morphology and is also particularly useful for identifying the neural or cancer stem cell population.
She explained how, like many academic researchers, she was using a few antibodies which she had many years of experience with. However, while these antibodies worked very well on the rat neurons she was using previously, they don’t always perform as well on human tissues. The other alternative, clinical antibodies from certified sources were reserved for use as a gold standard but they’re expensive for her research lab to purchase.
Dr. Tang-Schomer is currently working with BioLegend to find antibodies relevant to brain tissue, such as anti-Tubulin β3, anti-GFAP and anti-Nestin, for use in flow cytometry and immunohistochemistry.
"I need a large panel of antibodies which have non-overlapping spectrums. I tell BioLegend what antibodies I need and they tell me what antibodies are in stock which will provide a non-overlapping spectrum," Dr. Tang-Schomer explained.
Precision medicine has realized that every patient is different - we need to tailor our drugs to individual patients.
Future research directions
Dr. Tang-Schomer's research group has identified the cell culture protocols which allow them to successfully create personalized tissue cultures for the majority of the patient tumor samples they receive.
The research group is now looking for ways to streamline the work-flow to make it less manual and time-consuming for tissue engineers, which will allow the project to be scaled-up. Working with computer scientists and engineers, the group is hoping to design and build an automated machine to create the personalized cultures. This approach will allow the model to be utilized in large-scale drug screening or personalized medicine programs.
Another goal is to use the model to connect patient genetics to cancer treatment outcomes. Dr. Tang-Schomer hopes that in combination with genetic profiling of the patients, the model will be able to give insight into how individual genes can affect the success of treatment.
Dr. Tang-Schomer believes that the unique bioengineering approach she has coined in the field of neuroscience will continue to benefit the wider neuroscience research community, allowing them to create accurate cortical tissue models from various starting materials.
