Advances in CAR T Therapy: Reprogramming Patient Cells to Treat Cancer
Learn about the six steps of CAR T cell production and the technology ensuring optimal cell delivery to patients
25 Jan 2018
Chimeric antigen receptor modified T cell (CAR T) therapy is an emerging immunotherapy that involves the genetic engineering and ‘supercharging’ of patients’ own immune cells to treat their cancer. In this SelectScience® interview, Dr. Richard Jones, Senior Manager of Global Marketing, Particle Counting & Characterization Group, Beckman Coulter, describes the latest advances in CAR T therapy and outlines the important role that Beckman Coulter’s Multisizer cell counting and volume analysis technology has in the delivery of this novel treatment to patients.
Please introduce yourself and tell us about your current role.

I have a long-standing interest in the development and application of protein and cell analysis technologies. I trained at Harvard University as a Kirchstein postdoctoral research and teaching fellow and was then an assistant professor in the Ben May Department for Cancer Research at the University of Chicago. I led the development of protein analysis approaches for understanding the relationship of pharmacology, human genetics, and cell signaling networks in cancer.
Most recently, I managed a virology and microbiological testing contract research organization that performed custom testing of materials going into the manufacture of biopharmaceuticals.
As senior manager of global marketing at Beckman Coulter, I manage the commercialization of a series of cell and particle analysis instruments and track the pulse of the global cell and biopharma markets.
What are the most important areas in immunotherapy research right now?
Two important areas of cancer immunotherapy research that have shown great promise for treating cancer are immune checkpoint inhibitor therapies and chimeric antigen receptor modified T cell (CAR T) therapies. Immune checkpoint inhibitor therapies are more traditional types of therapy and involve the administration of small molecule or antibody-based therapeutics to reactivate the growth of immune cells that have been suppressed by cancer cells.
The new kid on the block is CAR T cell therapy, which involves the removal of a patient’s T cells, the genetic engineering of the cells to increase their ability to recognize the patient’s cancerous B cells, and then finally putting these supercharged T cells back into the patient. These T-cells are thereby programmed with the ability to specifically recognize a patient’s cancerous B cells and recruit the body’s immune system to destroy their cancer. Although early CAR T clinical trials encountered obstacles, more recent trials have been very successful by most metrics. Trials of a CAR T cell approach by Juno Therapeutics for acute lymphoblastic leukemia (ALL) in 2016 were ultimately halted due to several patient deaths related to neurotoxicity.
However, two CAR T therapies have now been approved by the FDA. The first FDA approved CAR T cell therapy announcement came in August 2017 from Novartis and was marketed as Kymriah. Kymriah is a therapy for adults and children with advanced leukemia. Patient responses to this therapy have been dramatically positive and many practitioners in the field of hematologic oncology are very optimistic about its potential.
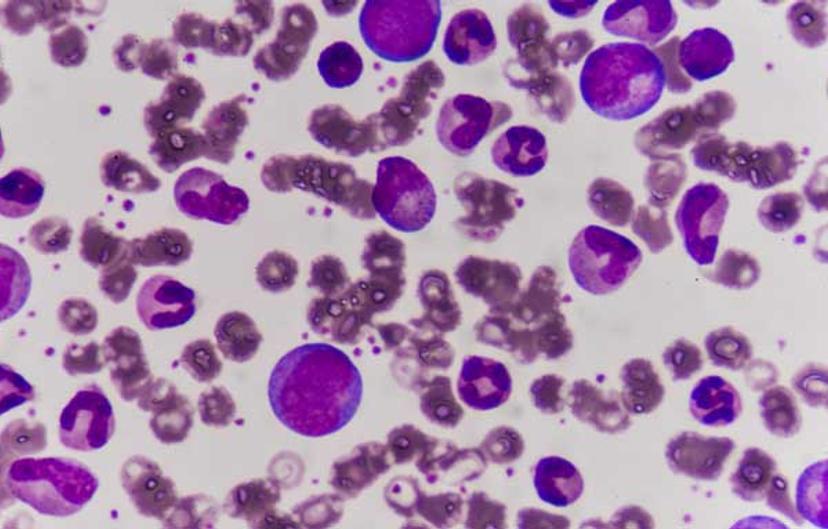
In October, Kite and its new parent company Gilead won the second FDA approval for a CAR T therapy with Yescarta. Yescarta is a CD19-directed, genetically-modified autologous T cell immunotherapy used to treat adults with relapsed or refractory large B-cell lymphoma. Diffuse large B-cell lymphoma (DLBCL), primary mediastinal large B-cell lymphoma (PMBCL), high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma (transformed follicular lymphoma, or TFL) fall into the class of cancer types treatable by this therapy. The approval of Yescarta was supported by data from the ZUMA-1 trial where 72 percent of patients treated with a single infusion of Yescarta responded to the therapy. 51 percent of patients had no detectable cancer remaining.
Both the Kite and Novartis therapies provide the possibility that patients who would otherwise have run out of treatment options, might now lead a cancer-free life.
How is the Beckman Coulter Multisizer used in CAR T cell therapy research and what are the main benefits of this technology for this application?
The process for making CAR T cells can be divided into six basic steps:
Blood collection, known as apheresis
Enrichment of T cells by methods such as centrifugation or antibody bead separation
Gene modification to introduce the chimeric antigen receptors to the T cells
Activation and expansion of the T cell population
Quality assessment of the activated cells
Formulation, delivery, and administration of the cells to the patient
The Beckman Coulter Multisizer is critical during the activation and ex vivo expansion step of CAR T production. Following gene modification, the T cells are activated by either antigen presenting cells or by beads that present antigens.

Following activation, the cells begin to proliferate and swell in volume until they reach an optimal size at which time they are assessed for quality and delivered to the patient. The Multisizer is used at the expansion step to monitor total cell count and cell volume to know when they are ready for delivery to the patient. Unlike imaging-based techniques that track the size of cells in two dimensions, the Multisizer measures the volume of cells that pass through a small hole in an aperture tube. When the cells pass through the hole, they displace a volume of electrolyte equal to their volume. Because volume is a cubed function of cell radius, it is a much more precise measure of cell size than cell area. Because cell counts and cell volume are critical parameters for CAR T therapy, the Multisizer is used here.
What do you see for the future of CAR T therapy?
There are two basic models for delivering CAR T therapy to a patient. In the first model, the processing of CAR T cells takes place in or close to a hospital. In the second model, the cells are shipped offsite to a remote cell manufacturing facility and then transported back to the hospital. It is not clear at this point which will predominate. However, it is clear that cell counts and volumes will continue to be critical quality attributes for the therapy in the future and the Multisizer will continue to play a central and vital role there.
Get more articles like these directly into your inbox. Sign up to SelectScience.


