Automation advances stem cell culture and differentiation for retinal disease research
Hear how the Ocular Tissue Engineering Laboratory is addressing retinal cell culture challenges via an automated stem cell robot platform
17 Apr 2025

Dr. Samuel McLenachan, Lions Eye Institute
Vision loss due to genetics or aging affects millions worldwide. Inherited retinal diseases impact approximately 1 in 4,000 people, with over 260 associated genetic mutations identified to date. Comparatively, degenerative retinal diseases account for roughly a quarter of blindness cases with age-related macular degeneration affecting around 8 million people globally. As our population ages, these numbers are expected to rise.
While most causes of vision loss have no cure, treatment options focus on slowing progression or improving quality of life via low vision aids and retinal prostheses. Dr. Samuel McLenachan, Senior Scientist at the Lions Eye Institute, Perth, Western Australia, hopes to improve this. As co-founder of the Ocular Tissue Engineering Laboratory, his work focuses on developing cell and gene therapies for incurable retinal diseases, including age-related macular degeneration, retinitis pigmentosa, and a range of other inherited retinal disorders. For his work to be successful, he relies on advanced cell culturing methods.
Challenges with retinal cell culture
Creating induced pluripotent stem cells (iPSCs) from somatic cells and then differentiating them into the cell, tissue or organoid of choice has become an important tool in research and drug development. However, creating retinal materials from iPSCs has historically proved challenging.
The retina is a complex tissue made up of six cell types in ten different layers, and to mirror its function in vitro requires the cells to be in the correct location and interact with each other in a specific way. This necessitates a variety of intrinsic and extrinsic factors and many different steps, meaning that manual methods to culture the required retinal tissue and organoids is a lengthy and labor-intensive process that does not lend itself well to scale-up.
Dr. McLenachan’s team has been working to create and culture retinal organoids and retinal pigment epithelial (RPE) cells. In order to develop the robust, reproducible, and efficient process needed for large-scale research, the team at the Ocular Tissue Engineering Laboratory has set up a collaboration with Tecan, a Swiss company with a focus on healthcare innovation including automation solutions.
The power of automation in cell culture
Automation reduces the amount of ‘hands-on’ work needed for cell culture, which frees up staff for other tasks and lowers the risks of contamination. More importantly, it reduces the possibility of human error, therefore increasing the reproducibility and reliability of results.
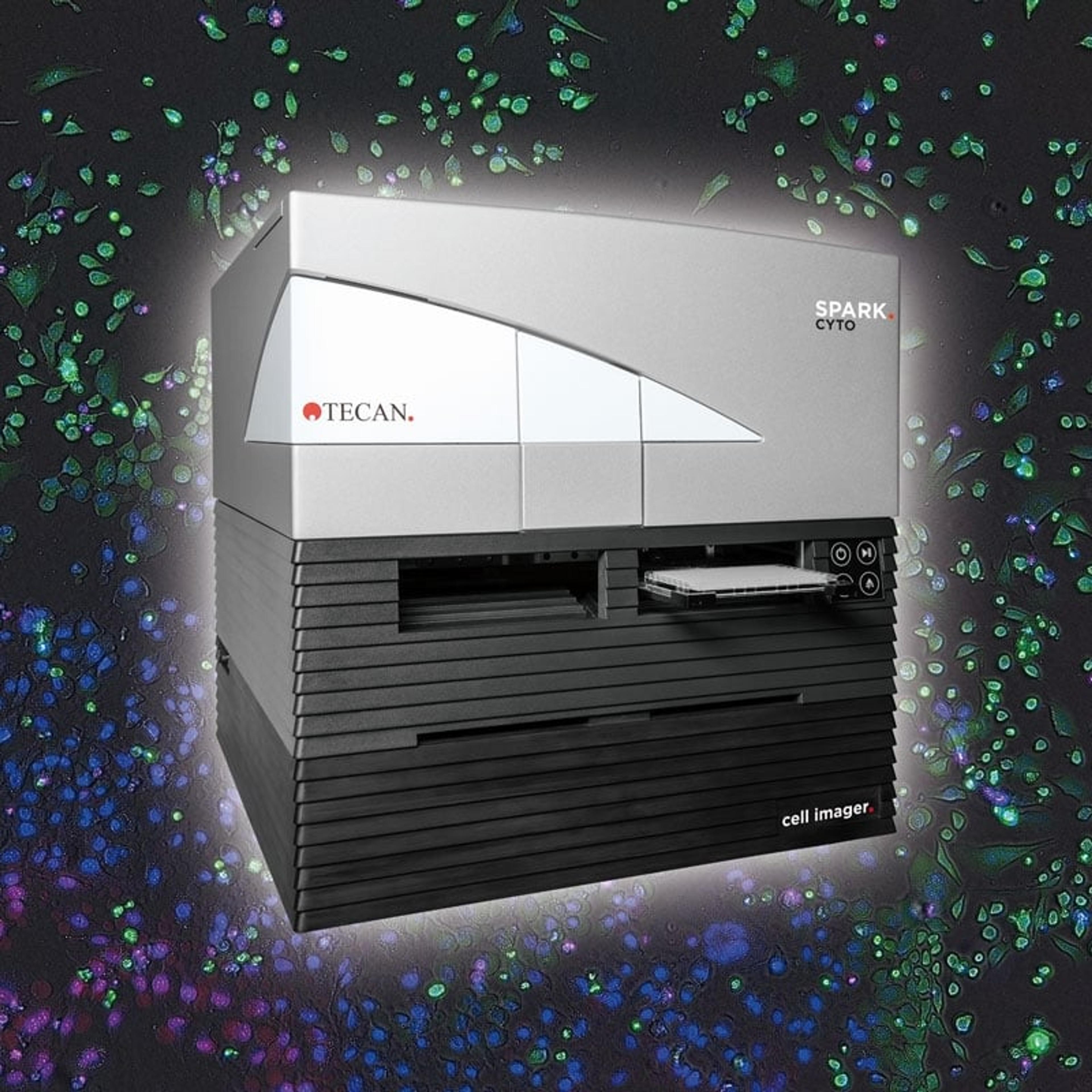
Dr. McLenachan and his team have collaborated with Tecan to create a stem cell robot platform and automated workflow for high-throughput cell culture. This was designed to culture patient fibroblasts and iPSCs, and then characterize and differentiate them into retinal organoids and RPE cells for drug screening applications. The stem cell robot, the first to reach Western Australia, incorporates Tecan’s Spark® Cyto automated imager for multimodal imaging of cell cultures and its Fluent® Laboratory Automation Workstation, which carries out automated media changes and drug treatments. The system also makes use of the Thermo Fisher Cytomat™ automated incubator.
Find out more and download the poster for free here.
“The system is managed with the FluentControl™ software, which uses drag-and-drop programming that’s very easy to pick up,” shares Dr. McLenachan. “It has a touchscreen interface for use by staff who don't have a full understanding of the system.”
Putting the platform to work
Using the stem cell robot platform, Dr. McLenachan’s team was able to culture dermal fibroblasts and iPSCs. Cell growth was demonstrated using phase contrast and brightfield images created by the Spark Cyto imager after a few days. The iPSCs were then seeded as single cells and cultured in a 96-well suspension culture plate. Again, using brightfield images, the researchers confirmed the formation and growth of embryoid bodies at days 2 and 16.
This setup was able to culture human retinal pigment epithelial cells derived from iPSCs that showed the development of pigmentation from weeks 5-6. Retinal organoids (RO) expressed photoreceptor progenitor markers CRX and RXRG at day 30 and RO morphology at day 49, as confirmed via brightfield imaging.
“We used the Spark Cyto imager multimodal imaging capabilities for IPS immunostaining showing nuclear OCT labelling in iPSCs, for luminescence assays in live adherent retinal organoids, and to confirm pigmented polygonal cell morphology in RPE monolayers,” explains Dr. McLenachan. “We’ve also established methods for assessing photoreceptor uptake and rhodopsin degradation.”
A platform for high-throughput screening
Drug discovery can be a complex, costly, and lengthy process. High-throughput drug screening allows drug developers to kickstart the process by selecting potential drug candidates rapidly from libraries of hundreds or thousands of possible molecules.
“To demonstrate the use of the stem cell robot platform in high-throughput screening in retinal disease, we carried out the largest drug screen our lab has ever done,” said Dr. McLenachan.
The proof-of-concept study involved treating 10-week iPSC-RPEs derived from a patient with RCBTB1-retinopathy in 16 96-well plates with a library of 283 FDA-approved antioxidant drugs (Selleckchem) over 24 hours. The researchers were able to measure reactive oxygen species and cell death in the live cells for all 283 drugs, using Thermo Fisher assays and fluorescence readings from the Spark Cyto imager, confirming its potential in drug screening.
Accelerated retinal disease research for a brighter future
Retinal disease research can be challenging. There are a lot of forms of disease, caused by a wide variety of factors, including many different gene mutations. These diseases can be complex or multifactorial and may affect only small populations.
By making the processes of cell culture and manipulation simpler, more robust, and more reproducible, automation can further advance retinal disease basic research. It can also help drug developers to select the best leads for therapeutic discovery, getting new and better therapeutics and diagnostics for unmet medical needs into the hands of physicians and patients more quickly. By using patients’ own cells as source material, it also has the potential to support personalized treatment options, such as cell and gene therapies. These benefits won’t just change the face of treatment for retinal and other eye disorders, they could make a difference across many different therapeutic areas.
Spark Cyto is for research use only. Not for use in diagnostic procedures.