Cellular models of disease: Trends in phenotypic screening
Paul Andrews, National Phenotypic Screening Centre, discusses challenges and trends in cellular modeling of disease
4 Nov 2019

Launched in 2015 in Dundee, Scotland, the National Phenotypic Screening Centre (NSPC), provides a collaborative approach to advance the drug discovery pipeline through cell-based phenotypic assays.
In this interview, SelectScience speaks to Dr. Paul Andrews, Director of Operations at NSPC, to learn about the key challenges and trends in cell-based phenotypic screening, the technologies advancing the field and some of the center’s innovative projects that are helping to identify lead candidates.
Plus, a sneak preview of Dr. Andrew’s ELRIG Drug Discovery 2019 session, Cellular Models of Disease, taking place on Tuesday, November 5 and Wednesday, November 6, at the ACC Liverpool, UK.
Tell us about the goals of the National Phenotypic Screening Centre
The idea of establishing this state-of-the-art phenotypic screening operation, was to try and redress the balance of ways that drugs were discovered. We decided to have a dedicated center focusing on cell-based, phenotypic assays, and to try and push the boundaries of what can be done technically.
We have a tripartite academic agreement, which allows for collaboration with industry partners. This is important because we wanted to build a bridge between the academic/clinical communities and the industrial community; where we talk the same language as the academics, but also talk some of the same language as the industry partners. The Phenomics Discovery Initiative (PDI), brings those two things together to develop high-quality biology into a high-throughput assay, using our industrial standard platform, which can be then exploited by the academic and/or industrial partners.
The goals are really to use the setup we have, which is mainly using microscopy and flow cytometry, to build assays that are predictive of human diseases, then execute those on different screening size libraries. One type of library is a toolbox library where we've got drugs, bioactive molecules or probes which have a known target. If we get a hit in those, then we know that those are potentially exciting as they changed the phenotype and we might know something about the target pathways involved, allowing an academic to test any of their hypotheses about what that disease biology is relevant to.
Once that's validated and we know that the assay is a robust screening approach for small scale, 3000-4000 compounds, we then decide whether to scale that up to a larger library of maybe 80,000 compounds or 100,000 compounds. This will then give lots of start points in medicinal chemistry.
We try and emphasize that assays should be as human as possible, using patient material if possible. Imaging, which is a very powerful tool for understanding cell behavior or flow cytometry, is also used. Since 2015, we've been working with Janssen Pharmaceutica in this PDI partnership, and we hope to have another biotech company starting at the end of this year.
The main thing is that we accelerate human biology understanding and the chemistry that goes with that program; whether that's a chemical biology tool or a drug. We've had assays in from mesothelioma, brain cancer, inflammatory diseases, neurodegeneration immuno-oncology, serpinopathies and we've got a very complex bronchial model for antiviral drug discovery. You can see we've got a wide range of different things which we drive forward.
What are some of the current challenges associated with cell-based assays for phenotypic screening?
Some of the challenges have to do with squeezing the biology into the multi-well format.
It's also things like co-cultures - two different cell types exist in the body, but we don't understand how the local milieu in the body allowing their co-existence can be transferred to an in vitro test platform.
When using stem cells - if you're deriving a cell from the stem cell, do you know that it's actually reproducing the phenotype of the cell when it's actually in the body? That could relate to the identity of the cell type or the maturity of the cell type. For example, a lot of neurons or cardiac cells that derive from stem cells in the lab aren't quite the same as they would be in the human body.
If you're doing a test in vitro, then you need to know how to age cells - how to recapitulate the types of insults that the human cell would get over a period of time - and how relevant it is, especially in the brain. How do you allow for donor-to-donor variation and achieve the miniaturization that's required from very low amounts of patient material?
A lot of people work on mouse systems because they're genetically amenable and, with the appropriate ethical approval, use them for in vitro and in vivo experiments. But lots of things don’t translate to humans as people have found, especially in areas such as neurodegeneration and the immune system. Laboratory mice exist in a quite sterile environment. We know now that the microbiome plays an important role in how therapies work, so that's another challenge to understand - whether the models that we use are the correct models.
One of the key criticisms of phenotypic screening is that you don't know what the target pathway is that you've engaged. You can start to use CRISPR screening in parallel to using target-specific small molecules and try to compare the phenotype of the cell treated with the target-specific probe to the gene knockout in pathway components. But ultimately, you probably do have to find the target pathway or the single target. The challenges around that are finding what that target is, whether proteomically or genetically.
What are the key trends in methods and technologies that will help overcome challenges in phenotypic screening?
We're using almost the best equipment that you can buy off the shelf. We use fast microscopes – confocal with multiple cameras - to look at the different things that can go on in the cell, but ultimately that's not enough. Technologies like imaging mass spec, which we don’t use yet, would be great to image a piece of tissue and work out the complexity of individual cell types.
We do diverge into unusual formats, like the Transwell format, and we've considered using microfluidic devices for certain applications. Although we don't currently use those; we collaborate with others that are exploring that.
We're also starting to use machine learning and artificial intelligence more often, especially in interpreting imaging data, and hopefully, through partnerships, in the drug design phase.
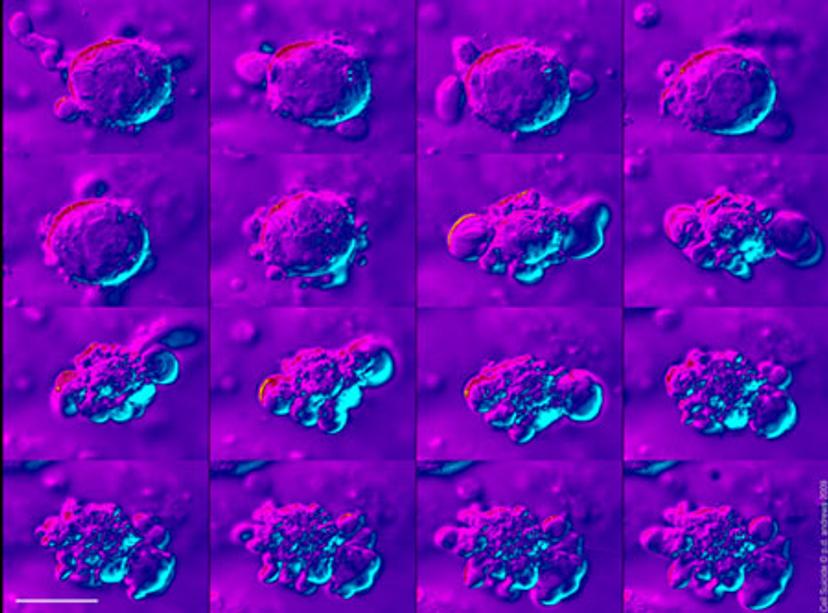
All these things will start to come together, and we’ll use multiple techniques going forward, especially when looking at large structures such as organoids or very small structures within the cell that might be dictating phenotypes.
The new technologies that we'd like to see implemented are things like light-sheet microscopy - to be able to look through larger objects in more complex biological systems in detail. With multimode imaging one could perform multi-scale analysis (from the nano- to the macro-scale) in high- or medium-throughput, or using fluorescence lifetime FRET-type imaging to measure things like protein-protein interactions within the cell in higher throughput.
We don't currently do any single-cell transcriptomics, but it is a very exciting way of adding additional descriptors that define a phenotype: we hope to get into this area in the future.
Quantitative proteomics is also a very important tool for understanding phenotypes and correlating it with the protein composition of cells. Another technology, which we don't use but is very exciting, (and will be covered in this ELRIG conference), is PROTACS which involved the targeted destruction of proteins, potentially allowing the removal of even the hardest-to-drug targets.

Tell us a little about the session you will be chairing at ELRIG Drug Discovery
The session that myself and Rob Vries of Hubrecht Organoid Technology have organized will cover the whole spectrum of cell-based assays relevant to disease, all the way from looking at cells to organoids.
We’ll hear from Prof. Steven Pollard from the University of Edinburgh, who collaborates with us on a patient-derived glioblastoma project, and Wendy Rowan from GSK, who will talk about a number of ways that GSK is trying to humanize the drug discovery pipeline all the way through to including organ-on-chip.
We also have some talks from people working on the cutting-edge of organoid biology, not just in the characterization of them, but also in the application of organoids for predictive purposes such as drug discovery or patient stratification. Rob Vries and Bon-Kyoung Koo, of the Institute of Molecular Biotechnology (IMBA), Vienna and Florijn Dekkers of Princess Maximina Center for Pediatric Oncology, Utrecht, will talk about, various aspects of what they're doing in their own labs, some of which is advancing technologies to do with, for instance, CRISPR screening in tumor organoids or intestinal organoids and also using imaging technologies.
I will also provide a retrospective of drug discovery - a reflection on what has gone on in the past, what worked and what didn’t, and then looking to the future. Together the talks will allow scientists at different levels to either see what's coming up or how they can apply organoid technology and cell-based assays into their research and drug development models in discovery pipelines.
What will you be working on next?
We've got a big project to find a male contraceptive. A few years back, the Bill & Melinda Gates Foundation put out a call to try and kick start new research on contraceptives. Of course, there aren't currently any male contraceptives on the market. There are a few clinical trials for hormonal-based contraceptives, but there are no non-hormonal male contraceptives. We recently secured funding for a multi-partner project to find lead candidates for a new male contraceptive. So that's quite an unusual project, to say the least.
We also have other projects in the pipeline to look at the genetic diversity in human populations and how that impacts the way drugs interact with their cells. We have partnered with other groups where we've got access to a bank of human-induced pluripotent stem (iPS) cells. We’re looking at profiling hundreds of drugs against iPS cells, either in the pluripotent state or in different states of differentiation. This work could have an impact on personalized medicine and help improve our understanding of the way that drugs interact with individuals across the population.
Register your place for ELRIG Drug Discovery 2019 and read more about trends in cell-based assays in the SelectScience Special Feature.
