Could organ-on-a-chip models help replace animal drug testing?
As the FDA and NIH plan to phase out animal-based drug testing, organ-chip models are filling this critical gap
14 Aug 2025
For decades, the pharmaceutical industry has relied on animal models for preclinical drug safety and efficacy studies. But, with rapid advances in human-relevant technologies, this field is on the verge of a major transformation.
In April 2025, the US Food and Drug Administration (FDA) announced plans to phase out animal testing in monoclonal antibody development and small molecule drug programs. Just last month, the National Institutes of Health (NIH) followed suit with a commitment to end funding for animal-only research and prioritize human-relevant approaches.
For R&D teams across the pharmaceutical and biotech sectors, the implications of these announcements are profound. In the next three to five years, animal studies are expected to become the exception rather than the norm. For developers, this means looking to alternative human-relevant models and learning how to adopt them.
The path to animal-free drug development

Dr. Lorna Ewart, Chief Scientific Officer, Emulate
According to Dr. Lorna Ewart, Chief Scientific Officer at Emulate, the steer from the FDA and NIH isn’t just an ethical decision, it’s a practical one. “It’s a recognition that animal models don't always translate into the clinic,” she says. Traditional animal models often fail to reflect critical aspects of human biology, leading to late-stage failures in safety or efficacy. “With the rise of more human-specific technologies, like cell and gene therapies, animal models are even outdated in some cases,” she adds.
While the FDA has long expressed interest in non-animal alternatives, what makes its latest announcement historic, is the introduction of a practical roadmap, a framework for integrating new approach methodologies (NAMs) into investigational new drug (IND) submissions. Among the alternatives highlighted are organ-on-a-chip models, a technology that Emulate has spent more than a decade advancing.
“It's a very significant moment for this entire space,” says Dr. Daniel Levner, Emulate’s Co-founder and Chief Technology Officer. “The FDA's announcement reflects a recognition that the technology has hit a certain threshold, a certain milestone, where it's now time for pharma to really engage with it.”
What are organ-chips?
Organ-chips are microfluidic systems that recapitulate in vivo cell and tissue microenvironments in an organ-specific context. They do so by culturing human cell types in a micro-engineered environment that recreates the natural physiology and mechanical forces—such as shear stress and peristalsis—that cells experience within the human body. The resulting platform not only mimics human physiology more closely than traditional cell culture but also allows researchers to observe functional responses often missed in animal studies.
Crucially, organ-chip technology has advanced well beyond proof-of-concept. Emulate’s products have been used by the scientific community to create over 30 organ models across more than 130 peer-reviewed publications. Its flagship model, the Liver-Chip, offers a powerful tool for drug safety and toxicity testing that has already outperformed traditional animal models.

Dr. Daniel Levner, Co-founder and Chief Technology Officer, Emulate
“In a 2022 study, we evaluated the predictive capabilities of the Liver-Chip using a blinded panel of 27 drugs with known clinical outcomes,” explains Levner. “We were able to capture 87% of hepatotoxic drugs that were missed by prior animal testing. And the system had 100% specificity, meaning that we didn't erroneously say that a drug was toxic that wasn't.”
The benefit for developers is not just reduced risk but also cost. An economic analysis included in the study estimated that organ-chips could save large pharmaceutical companies $100–150 million annually, simply by enabling better early-stage decisions.
“Another good example is our collaboration with Moderna,” adds Levner. “They evaluated the Liver-Chip as an alternative to non-human primate studies for lipid nanoparticle development. Their analysis showed the approach could cut study costs by up to 94% and reduce timelines by 70%.”
Turning FDA guidance into reality
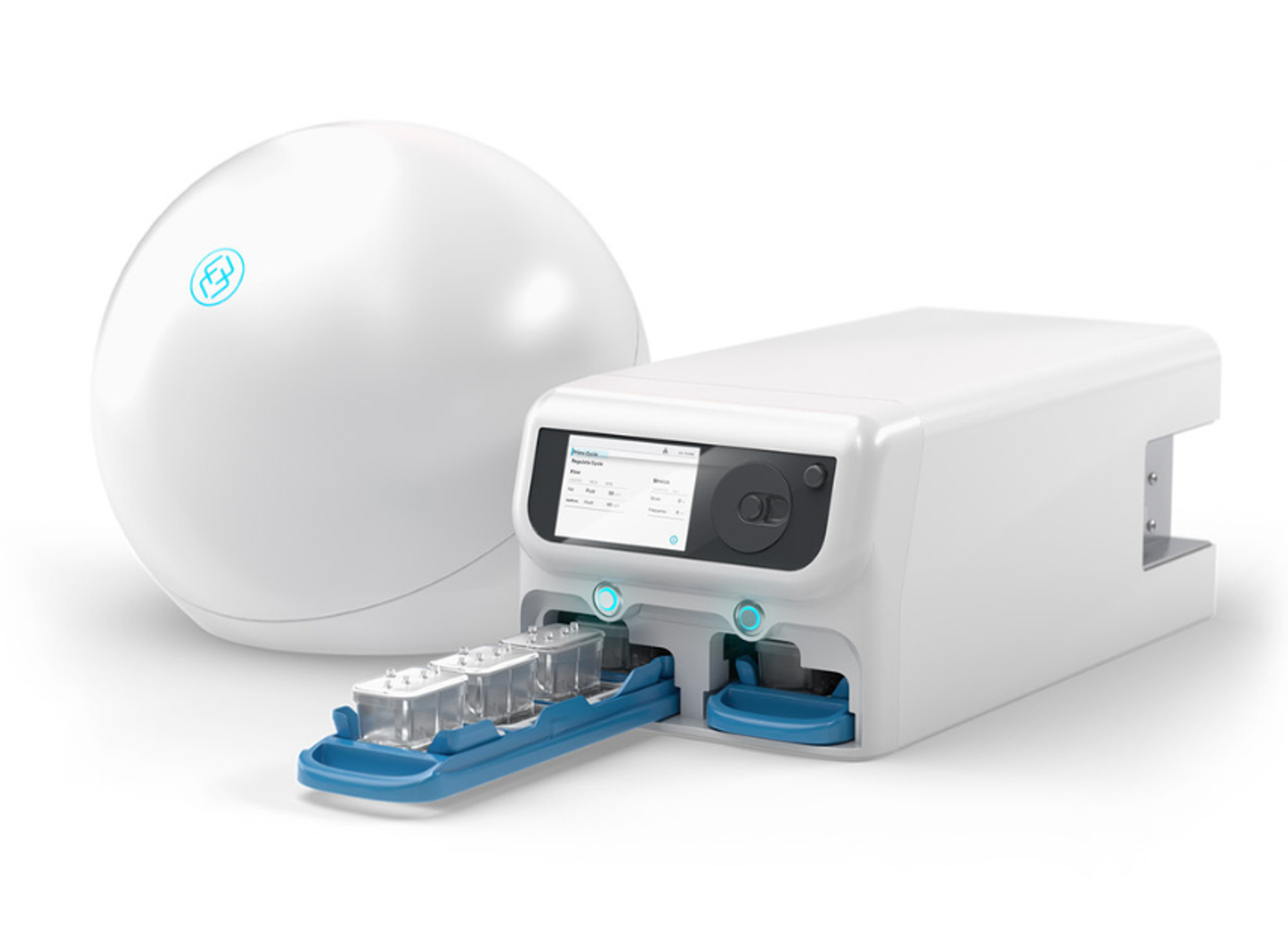
Emulate’s organ-chips have been on the FDA’s radar for nearly a decade. After launching its first-generation Zoë platform, the company entered a cooperative research agreement with the agency. The work soon expanded across five FDA labs and included models for the liver, lung, intestine, brain, and alveolus.
Most recently, Emulate’s Liver-Chip became the first and only organ-chip technology accepted into the FDA’s ISTAND program, which aims to qualify new drug development tools for regulatory use. The submission focuses on its ability to predict drug-induced liver injury (DILI) – a common reason drugs fail in development.
“The Liver-Chip allows researchers to compare a candidate’s hepatotoxicity risk relative to other drugs in the same class,” explains Levner. “It’s not binary – toxic or non-toxic – it produces a quantitative score, correlated according to the severity of DILI.”
“The DILI scores not only can correlate to severities based on historical datasets but can also allow users to rank order their molecules in development,” adds Ewart.
This is where she sees the Liver-Chip being immediately used, as a screening tool before in vivo dose finding studies. “At this stage of development, teams often have two or three promising compounds. Using the Liver-Chip, researchers can assess each one’s potential for liver toxicity and make more informed decisions about which to progress,” she says. This translates to fewer animal studies, lower costs, and a higher likelihood of success in first-in-human studies.
“Beyond toxicology testing, many of our customers are now using these organ-chips in the efficacy domain and even target validation studies,” she adds.
The platform’s microfluidic design also opens possibilities for studying drug delivery mechanisms. “Because our systems use two parallel channels, we can, for example, apply a drug to the vascular side lined with endothelial cells and observe whether it crosses into the epithelial tissue to reach its intended target,” says Ewart. “There are numerous different ways that these chips can be implemented, and I'm excited to see what people's imagination leads to.”
Introducing AVA
To expand those possibilities even further, Emulate recently unveiled AVA, a new platform designed to build on the foundation established by its first-generation system, Zoë.
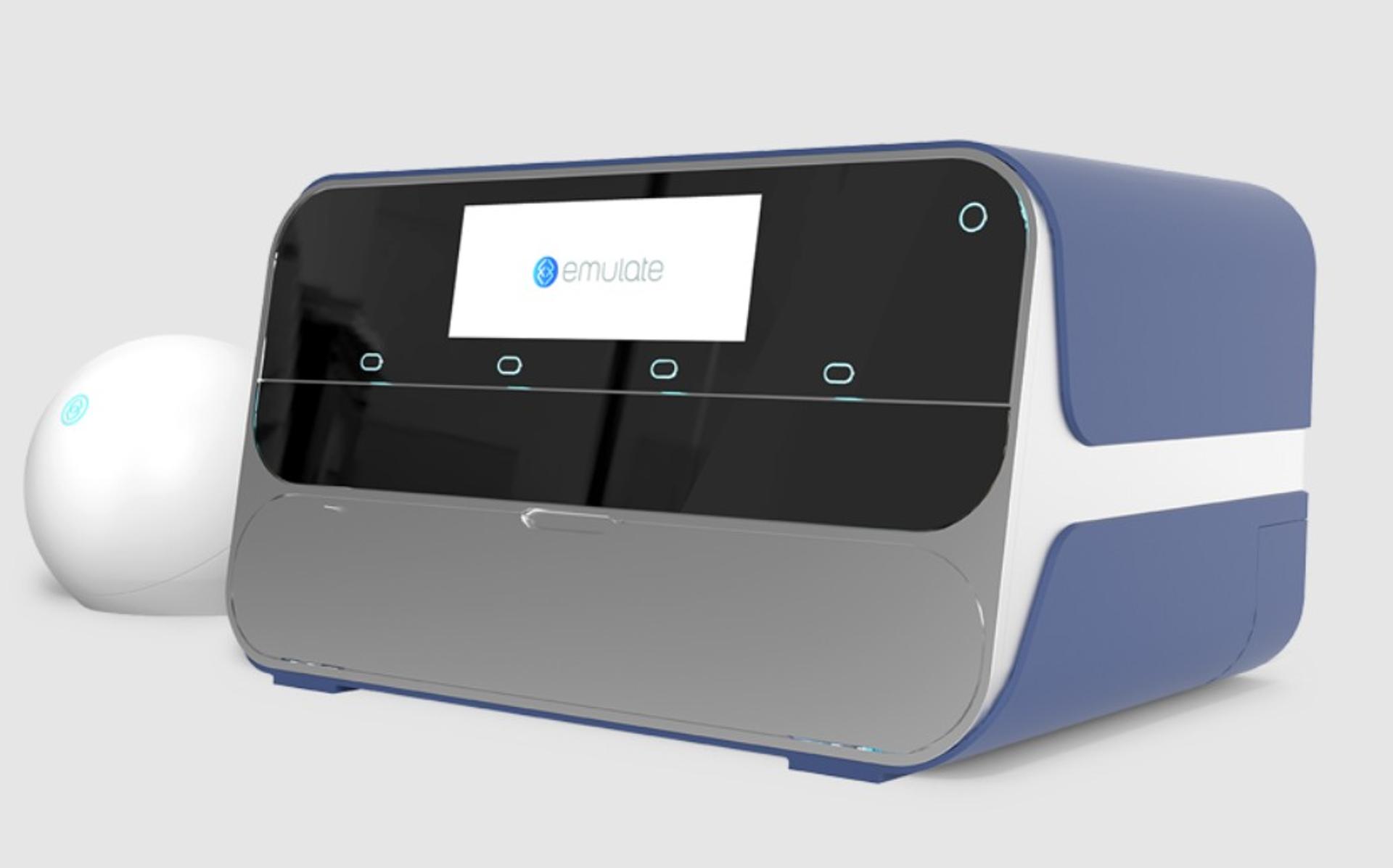
“Like the FDA announcement, AVA represents a new threshold that organ-on-a-chip technology has now reached.” - Dr. Daniel Levner
AVA is the first self-contained organ-chip workstation to integrate high-throughput tissue culture, full environmental control, and real-time imaging in a single benchtop unit. “It’s a self-incubated system, which saves lab resources, and it includes an automated microscope, because inspecting chips manually was a significant time burden,” says Levner.
AVA can run up to 96 emulations simultaneously, compared to Zoë’s 12. It also uses half as many cells and media per sample. “Critically, it reduces hands-on scientist time by as much as two-thirds,” Levner adds.
Where to start
While the shift away from animal models is widely welcomed, turning that ambition into practice is far from straightforward. How can developers begin integrating alternatives like organ-chips without disrupting established in vivo workflows? Levner suggests starting small. “It doesn’t take much to begin running parallel studies. The technology is relatively easy to adopt, and in some cases, there are facilities or partners who can run the models for you,” he says.
Ewart urges developers to start now. “For smaller companies that haven’t done anything in this space yet, now’s the time to get involved. Dip your toes in, see what kind of data is generated, and learn from it,” she says. “For those already experimenting with organ-chips, start thinking beyond parallel use to how to replace animal models where possible.”
Greater data transparency and data sharing will also be critical to build a robust evidence base for new approach methodologies (NAMs). “Understanding how different users in different laboratories are applying these methods – and showing that they can produce reproducible results – is key,” says Ewart. “Animal models have decades of standardized data behind them. To gain similar trust, we need to build up an equivalent body of shared evidence for organ-chips and other promising alternatives,” she concludes.