Enhancing quality in clinical laboratories with Six Sigma
Guest editorial by Mark Holland, Ph.D. Director, Bioinformatics/Biostatistics for Chemistry and Immunoassay Research and Development, Beckman Coulter
10 Nov 2024
©wrightstudio @123rf.com
In the fast-paced world of clinical laboratories, accuracy and precision are of utmost importance. The sigma metric has emerged as a valuable tool for assessing assay performance, comparing instruments, and optimizing quality control schemes. Learn more about the impact of Six Sigma in enhancing quality and reducing errors.
Why is Six Sigma important?
According to Dr. Mario Plebani, a leading voice in laboratory medicine and quality,1 analytical quality is achieved by “setting and implementing evidence-based analytical quality specifications in everyday practice.”2 Measuring how far tests and processes deviate from perfection is done by implementing Six Sigma methodology. Six Sigma has proven to be highly applicable in the field of diagnostics to enhance quality. By applying statistical analysis and process control tools, Six Sigma helps laboratories measure, analyze, and optimize diagnostic processes, increasing efficiency and improving patient outcomes. Integrating Six Sigma principles into diagnostic quality is valuable for laboratory directors to systematically identify and eliminate defects for both assays and analyzers,3 empowering laboratories to identify quality products and ultimately ensure high-quality diagnostic services.4
What goes into sigma metric?
The sigma metric in clinical laboratories provides a quantitative assessment of assay performance. The sigma metric in the clinical laboratory for an analyte or test is calculated using three variables that are routinely available:
- Imprecision (SD or %CV)
- Inaccuracy (Bias)
- Allowable total error (ATE / TEa)5
The sigma metric measures the number of standard deviations between the assay’s mean and the nearest allowable total error limit. A higher sigma metric indicates better performance, while a lower sigma metric suggests a higher error risk.
What is precision?
The summarized data from routine quality control (QC) testing over time can be used to determine a cumulative coefficient of variation (%CV). The Clinical and Laboratory Standards Institute (CLSI) recommends a period of several months or more for this analysis, as stated in CLSI Document C24, 4th ed. To assess precision, which measures the random error in measurements, CLSI guideline EP05-A3 suggests following a 20-day protocol. This involves testing controls twice per day with a minimum of two hours between runs for 20 days. It is important to generate precision data at various analyte concentrations, as analytical performance can vary across the reportable range. Lower concentrations often exhibit higher CV values, except for assays especially developed for high sensitivity. Precision should be evaluated at a concentration close to a medical decision level. If this is not possible or available, concentrations within the normal reference range and at a pathological concentration should be evaluated. Manufacturers' controls and commercial QC are often set close to these limits.
What is inaccuracy bias?
Bias is the systematic difference between the generated result and the expected result. It can be categorized as either true or relative, depending on how the expected result was obtained. True bias can be determined through reference methods, reference materials, proficiency testing, or external quality assessment surveys. Peer group mean can also be used to assess bias. Relative bias is determined through comparison studies between methods, instruments, or reagent lots. It is important to note that bias may vary depending on the concentration of the analyte.
What is total allowable error (TEa) / allowable total error (ATE)?
TEa (or ATE), an essential concept in healthcare laboratories, combines the imprecision and inaccuracy (bias) of a method to limit the total impact on a test result. It represents the allowable total error that can be tolerated in a test result without negatively affecting patient care.
Proposed TEa values for different assays can be obtained from recognized sources like CLIA,6 Dr. Carmen Ricos and colleagues EFLM Biological Variation Database,7 German Guidelines for Quality (RiliBÄK),8 and Australian RCPA.9 However, there can be significant variation in recommended TEa values among these sources, which can introduce uncertainty when interpreting and generalizing sigma metrics for different assays. This variation complicates head-to-head comparisons of assays from different manufacturers. To determine the appropriate quality for making medical decisions, it is crucial to consult clinicians in addition to considering published TEa values.
Precision (CV%), inaccuracy Bias (absolute value of Bias) and total allowable error (TEa) are commonly expressed as percentages.
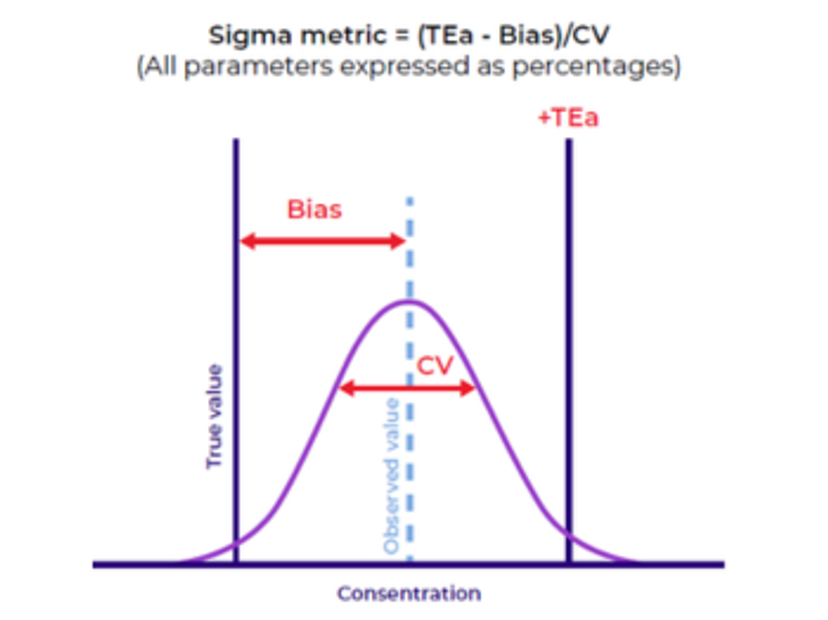
Figure 1. The relationship of imprecision (CV), inaccuracy (Bias) and total allowable error (TEa)10
Image provided by Beckman Coulter Diagnostics
Optimizing quality control (QC) schemes
One of the critical applications of sigma metrics is in designing optimal quality control schemes for individual analytes. By analyzing the sigma values for different analytes, laboratories can determine the appropriate frequency and intensity of QC measurements. This approach ensures that the necessary level of control is maintained while minimizing unnecessary QC testing, saving time and resources.
Reducing analytical errors
A high sigma metric directly correlates with a lower number of analytical errors. When a clinical laboratory operates at a high sigma level, there are fewer instances of questionable test results being accepted and reported. This means that clinicians can have greater confidence in the accuracy of the reported results, leading to improved decision making and patient care.
Minimizing false rejections
A high sigma metric reduces the number of acceptable results falsely rejected and not reported. False rejections can lead to delays in patient diagnosis and treatment, potentially compromising patient outcomes. By implementing robust QC schemes based on sigma metrics, laboratories can ensure that valid results are not mistakenly discarded, contributing to improved efficiency and patient care.
Levels of sigma11
Four: When a test achieves a sigma metric value of four, it means it has less than an estimated 6,210 errors for every one million actions.
Five: When a test achieves a sigma metric value of five, it means it has less than an estimated 233 errors for every one million actions.
Six: When a test achieves a sigma metric value of six, it means it has less than an estimated 3.4 errors for every one million actions.3,11
Here is an example of how it shows up:
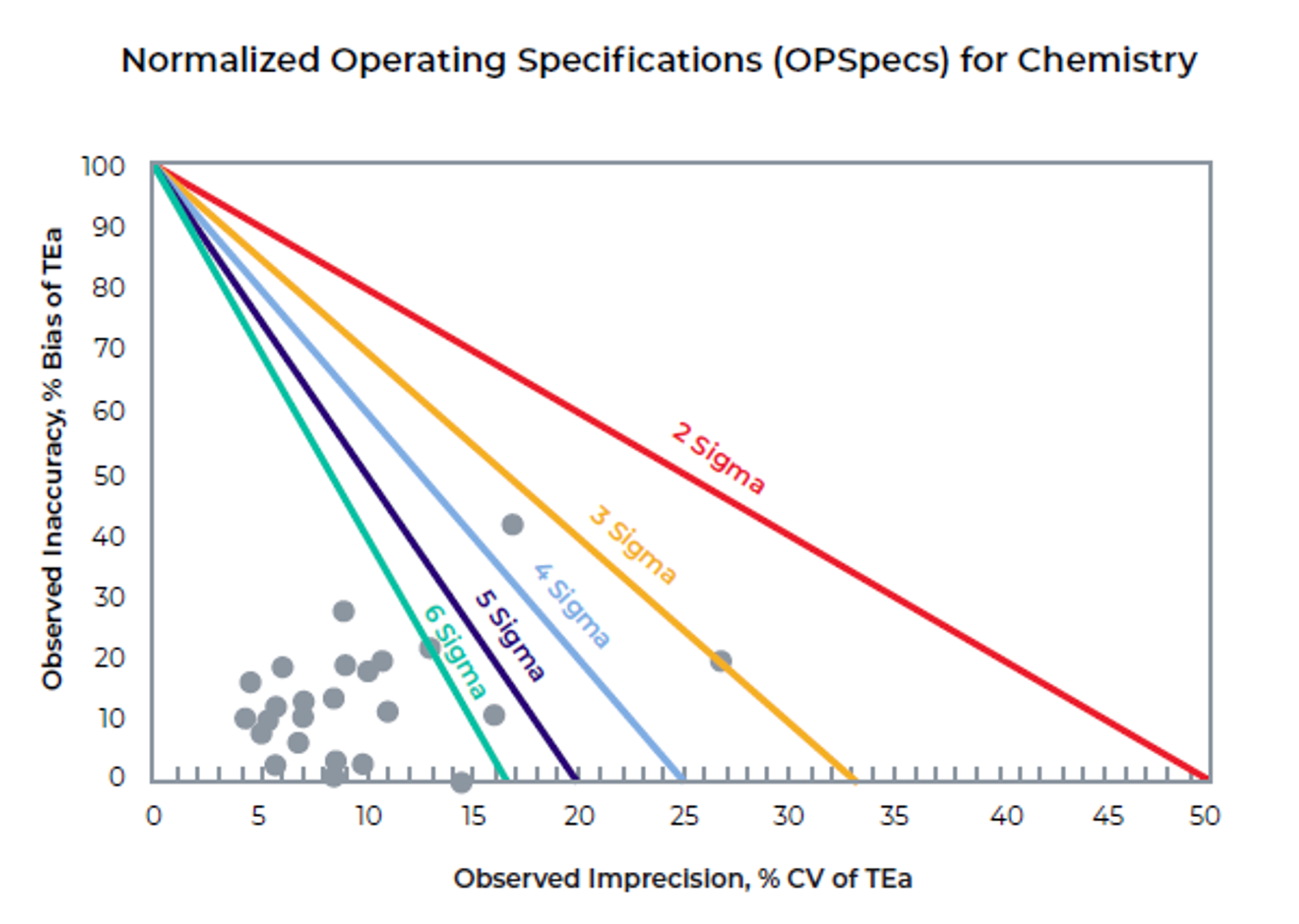
Figure 2. Normalized Operating Specifications for Clinical Chemistry Assays10
Image provided by Beckman Coulter Diagnostics
The normalized parameters are plotted and shown in the graph. The colored lines indicate the sigma metric (6, 5, 4, 3 and 2). For the 24 chemistry assays, 21 are 6 sigma or greater and are shown in the lower left corner of the figure. One assay is in the 5 to 6-sigma range, one is in the 3 sigma range, and one is in the 2 to 3 sigma range.
Application of Six Sigma in your laboratory
Combining sigma metrics with QC design tools allows laboratories to customize and optimize their quality control procedures, reducing waste and costs associated with inefficient QC procedures in terms of time and materials.
The Westgard group has developed one example of a QC strategy using sigma metrics. The Westgard Sigma Rules™12 incorporated the use of sigma metrics with the original Westgard QC rules.
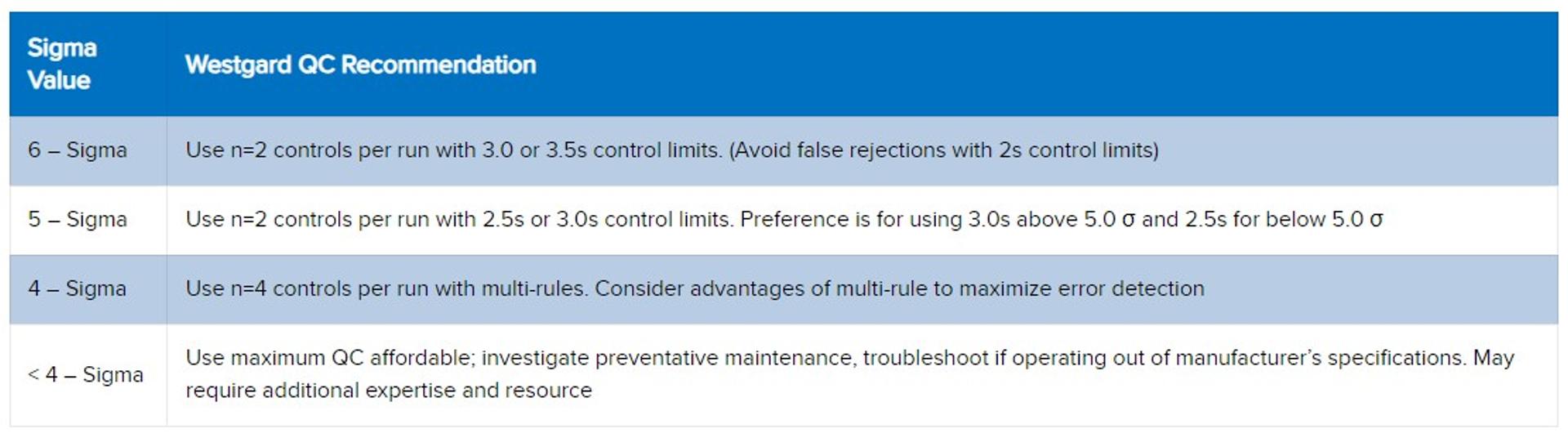
Image provided by Beckman Coulter Diagnostics
Use maximum QC affordable; investigate preventative maintenance, troubleshoot if operating out of manufacturer’s specifications. May require additional expertise and resource
Conclusion
Using Six Sigma, laboratories can identify and address sources of error, reduce variability, and improve overall diagnostic accuracy and reliability.13 Implementation of Six Sigma methodologies in clinical laboratories results in significant quality improvements, including reduced turnaround times, and decreased errors.3,14 By striving for higher sigma values, laboratories can enhance the quality of their test results, reduce analytical errors, minimize false rejections, and decrease the need for reruns and troubleshooting time spent by laboratorians on spurious results.15–18
Integrating Six Sigma principles into diagnostic quality is a valuable tool for laboratory directors to identify and eliminate defects, ensuring high-quality diagnostic services systematically. As technology advances and the demand for accuracy grows, the application of Six Sigma will continue to play a vital role in improving patient care and outcomes in clinical laboratory settings.
This blog post is shared as part of the global CLINICAL24 conversation. Visit the Innovation Hub to learn more about high-sensitivity immunoassay advances.
References:
1. Lippi G, Gillery P, Graeves R, et al. Mario Plebani turns 70. Clin Chem Lab Med. 2021;59(1):1-5. doi:10.1515/cclm-2020-1718
2. Plebani M. The CCLM contribution to improvements in quality and patient safety. Clin Chem Lab Med. 2013;51(1):39-46. doi:10.1515/cclm-2012-0094
3. Applying Six Sigma to Lab Quality Management Systems. Six Sigma Daily. June 15, 2020. Accessed January 5, 2024. https://www.sixsigmadaily.com/six-sigma-lab-quality-management/
4. Smy L. The Case for Six Sigma in Lab Quality Management Systems | myADLM.org. Association for Diagnostic and Laboratory Medicine. April 2020. Accessed January 5, 2024. https://www.myadlm.org/cln/articles/2020/april/the-case-for-six-sigma-in-lab-quality-management-systems
5. Westgard JO, Westgard SA. Total Analytic Error: from Concept to Application. Quality Requirements and Standards. September 2013. Accessed April 15, 2024. https://www.westgard.com/essays/quality-requirements-and-standards/622-ate-tea.html#goals
6. Westgard JO. 2024 CLIA Proposed Acceptance Limits for Proficiency Testing. Quality Requirements. 2023. Accessed April 16, 2024. https://www.westgard.com/clia-a-quality/quality-requirements/1002-2024-clia-requirements.html
7. EFLM. EFLM Biological Variation Database. Accessed April 16, 2024. https://biologicalvariation.eu/
8. Westgard JO, Westgard SA. Rilibak - German Guidelines for Quality. Quality Requirements. 2015. Accessed April 16, 2024. https://www.westgard.com/clia-a-quality/quality-requirements/439-rilibak.html
9. RCPA. RPCA Manual. 2024. Accessed April 16, 2024. https://www.rcpa.edu.au/
10. Shih J. USING SIX SIGMA METRICS TO MONITOR THE QUALITY OF RESULTS. 2016;(BR-51862).
11. Westgard S, Bayat H, Westgard JO. Analytical Sigma metrics: A review of Six Sigma implementation tools for medical laboratories. Biochem Med (Zagreb). 2018;28(2):020502. doi:10.11613/BM.2018.020502
12. Westgard JO. Westgard Sigma Rules. Westgard Rules. September 2014. Accessed April 16, 2024. https://www.westgard.com/lessons/westgard-rules/58-westgard-rules/661-westgard-sigma-rules.html
13. Westgard JO. Useful measures and models for analytical quality management in medical laboratories. Clin Chem Lab Med. 2016;54(2):223-233. doi:10.1515/cclm-2015-0710
14. Inal TC, Goruroglu Ozturk O, Kibar F, et al. Lean six sigma methodologies improve clinical laboratory efficiency and reduce turnaround times. J Clin Lab Anal. 2018;32(1). doi:10.1002/jcla.22180
15. Westgard S. 113 Improve Lab Operations with Six Sigma Metrics. In: 2011 Annual Meeting – Las Vegas, NV. ACEP; 2011.
16. Chawla R, Goswami B, Singh B, Chawla A, Gupta VK, Mallika V. Evaluating laboratory performance with quality indicators. Lab Med. 2010;41(5):297-300. doi:10.1309/LMS2CBXBA6Y0OWMG
17. Rathi R, Vakharia A, Shadab M. Lean six sigma in the healthcare sector: A systematic literature review. Mater Today Proc. 2022;50:773-781. doi:10.1016/j.matpr.2021.05.534
18. Westgard QC. Delnor Community Hospital Sigma Verification of Performance. Westgard. 2023. Accessed January 25, 2024. https://westgard.com/resources/130-sigma-verification-of-performance-program/991-sigma-vp-delnor-community.html

