Host response diagnostics gives new hope in AMR battle
Experts discuss the game-changing potential of novel host response-based diagnostics to combat the global challenge of antimicrobial resistance (AMR)
20 Dec 2023

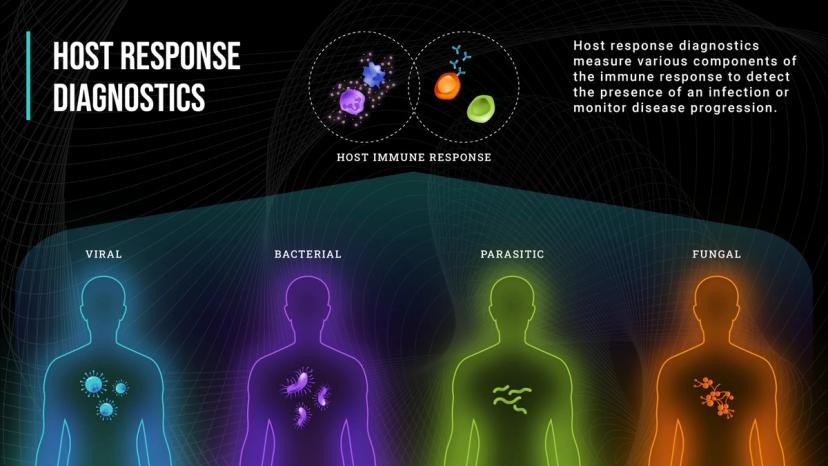
Host response-based diagnostics can transform conventional molecular diagnostics by distinguishing between viral and bacterial pathogens. This novel approach leverages the host-immune response and detects specific signatures of infection, enabling healthcare providers to optimize antibiotic use in point-of-care settings, helping to combat the worrying rise in antimicrobial resistance (AMR).
Speaking with Max Perelman, President and Chief Executive Officer, and Jesse vanWestrienen, Executive Vice President of Products at Biomeme, we explore the challenges of antimicrobial stewardship in point-of-care diagnostics, and unveil an innovative solution that's poised to make a significant impact for patients and healthcare providers alike.
Biomeme is leading the charge in the field of decentralized molecular diagnostics; an approach where testing and analysis of molecular markers takes place outside of centralized laboratory settings such as in a hospital or offsite reference lab. This method relies on the use of portable and point-of-care devices in diverse settings, from emergency departments to field clinics and even unconventional testing venues, to enable broader access to diagnostics and rapid molecular testing.
Fighting antimicrobial resistance with decentralized molecular diagnostics
Biomeme’s core mission reflects the company’s commitment to holistic health. JessevanWestrienen says, “our team wants to design and develop decentralized molecular diagnostics to ultimately help in achieving One Health – the idea that true human health goes hand in hand with the well-being of the planet, encompassing all life-forms as well as the diverse ecosystems.”
“The COVID-19 pandemic has catalyzed a shift in bringing molecular detection with different capabilities into people’s homes,” says Perelman. “Ideally, when a patient is unwell, they should not leave home to avoid the risk of potentially infecting other people. We should instead aim for a different patient journey, that looks like this: an initial telemedicine visit, followed by remote care guided by diagnostic data, eliminating the need for a physical consultation unless it’s essential. This is what our company’s goal is built around: to bring robust diagnostic capabilities into a point-of-care setting and eventually into homes, making healthcare more accessible and efficient by empowering individuals to perform personal diagnostics.”
One of the major hurdles in reaching this goal of One Health is the growing global challenge of AMR. AMR is especially prevalent in regions of low resource, where appropriate use of antimicrobials is often lacking. This is often a result of low-quality products, inconsistent adherence to treatment regimens, or a lack of awareness of the consequences of antibiotic misuse, compounding the spread of AMR.
Specifically, Perelman observes that respiratory diseases and sexually-transmitted infections (STIs), given their widespread occurrence worldwide, account for a large proportion of AMR cases. For example, resistance has appeared and expanded with every release of new classes of antibiotics for the treatment of gonorrhea, and strains of multidrug-resistant gonorrhea that do not respond to any available antibiotics have already been detected.
“This underscores the need for interventions to promote optimal antibiotic usage," asserts Perelman. “And with antimicrobial stewardship, it is crucial to consider diagnostics as well. When an infectious disease of unknown origin is presented at the emergency department, the clinical team is obligated to conduct comprehensive testing – from CT scans to PCR detection. Not only does this quickly become time-consuming and expensive, but it can also be invasive and disruptive to the patient.” Indeed, with AMR, the consequences to healthcare systems are multi-fold, adds vanWestrienen. “Antibiotic misuse inevitably increases healthcare costs. It results in unnecessary use of medical resources with increased visits to the clinic for the patient, prescription costs, and additional testing. Furthermore, as antibiotic resistance continues to grow, there is a real risk of entering a post-antibiotic era, where commonplace bacterial infections could evolve into life-threatening conditions. Thus, this becomes a question of the preservation of future antibiotic effectiveness.”
Addressing the shortcomings of conventional diagnostic methods
A new field of host response-based diagnostics has emerged, which holds the potential to solve many of the challenges with traditional approaches. “When it comes to distinguishing between bacterial and viral infections, healthcare professionals heavily depend on clinical assessment and patient history. However, this approach is not always accurate and can lead to misdiagnoses,” cautions vanWestrienen.
“Traditionally, clinicians utilize pathogen-based infectious disease diagnostics, such as PCR panels or sequencing-based diagnostics, targeting a limited set of pathogens," vanWestrienen continues. “Focusing solely on identifying specific pathogens limits the ability to identify emerging or rare infections, let alone achieve early detection. And while faster molecular tests are gaining in popularity, traditional pathogen-based detection methods involving long microbial culture times, prone to false positives, continue to be widely used.”
“Host response diagnostics rely on the host-immune response and the detection of specific host-response signatures for disease diagnosis,” Perelman explains. He highlights two noteworthy use cases for host response-based diagnostics that sets them apart from direct pathogen-based detection: “The first is in identifying challenging bacterial or viral infections. This is because some pathogens cannot be readily detected through minimally-invasive sampling, and not all viruses are included in some of the large pathogen detection panels commonly in use today. This means there are data gaps for the detection of some viral infections.”
“The second application of host response diagnostics is in monitoring a patient’s response to treatment, which is something that cannot be accomplished via pathogen-based testing,” continues Perelman. “This is particularly important in the context of AMR because clinicians are ultimately aiming to minimize the length of antibiotic use. Having a diagnostic tool to guide adjustments in antimicrobial therapies – such as transitioning from an IV-based therapy to a pill – could facilitate earlier patient discharge from hospitals. This outcome not only enables efficient bed management, it lowers the costs of healthcare services whilst also reducing potential exposure to hospital-acquired infections.”
However, host response as a concept is so new, caveats vanWestrienen, that just a handful of solutions exist in the market today. “Only a few companies have received US FDA clearance for commercial test use. All available host response tests rely on protein-based detection methods, targeting up to three markers at most,” he explains. “And further, the potential of host response remains untapped because, ultimately, protein-based tests lack the precision and sensitivity seen in molecular tests,” reveals vanWestrienen. He goes on to explain that the underlying reason is that in infected patients, some immune-related genes are upregulated leading to increased protein production, while others are downregulated, reducing protein output. Unlike molecular regulation which can be detected quickly, this creates a lag between gene expression and protein production and detection. Additionally, while molecular diagnostics, as an amplification technology, can selectively detect and amplify small amounts of a molecular biomarker, protein-based methods may not be sensitive enough to detect trace protein amounts.
A quick, affordable and accurate point-of-care molecular solution

The need for an inexpensive, minimally invasive, and complete host response-based diagnostic platform, especially one that is also designed to work in resource-limited areas, did not go unnoticed by the team at Biomeme. To address this, the team has developed the compact Host Response Test (HR-B/V) on its Franklin® ISP platform, which offers a comprehensive blood-based test focusing on 23 mRNA gene targets. Unlike conventional solutions that track only on a limited number of protein markers, the molecular basis of the HR-B/V test allows for increased sensitivity and accuracy, crucial in differentiating between bacterial and viral infections.
The key to getting the HR-B/V test to where it is today has been Biomeme’s long-standing relationship with LGC Biosearch Technologies, experts in oligonucleotide design and manufacturing. "We have used LGC’s support extensively, sourcing many custom oligonucleotides and primers from them, and have always been pleased with the consistently high product quality they deliver. Recently, when we had some challenges with one of our other suppliers, they stepped in and stepped up to help ensure we could deliver. Their technical support has been instrumental in helping realize our goal of a fast, affordable, accurate, and easy-to-use blood-based molecular detection platform,” mentions vanWestrienen.
To begin with, Biomeme’s portable test is aimed for use in critical care settings to provide emergency physicians with the data they need to aid informed decision-making within an hour or less of testing. Looking ahead, the Biomeme team envisions expanding its impact from emergency departments to outpatient and point-of-care settings. The goal is to reduce time to results to as low as 15 minutes, making diagnostics more efficient across healthcare settings including ambulatory and primary care.
Collaborations, such as that with LGC Biosearch Technologies, have played a crucial role in advancing Biomeme's host response-based approach to AMR and antibiotic stewardship. The team at Biomeme is actively engaged in clinical research as well as clinical studies and welcomes collaborators who share their commitment to revolutionizing the field of molecular diagnostics.
