Identification of Candida auris and echinocandin resistance-associated mutations
Candida auris (C.auris) infections are a major global health challenge, with nosocomial outbreaks on the rise and many strains exhibiting resistance to antifungal agents. New real-time PCR tests enable sensitive and specific identification of the pathogen and of the most important mutations associated with resistance to echinocandins (ECH).
21 Jun 2024
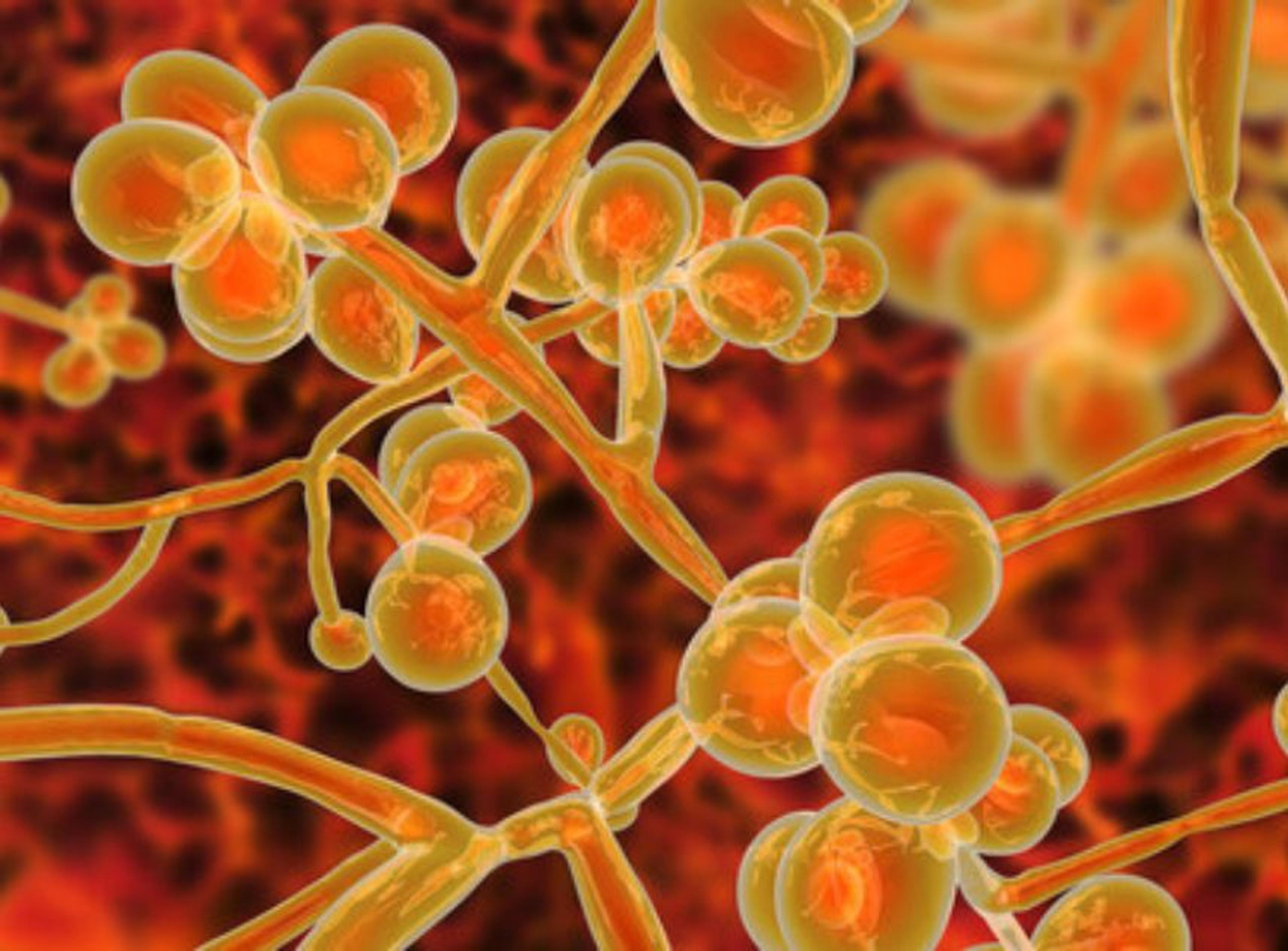
Emerging fungal infection
C. auris was first reported in 2009 in Japan and is now spreading rapidly worldwide. Many strains are resistant to common antifungals and the increasing occurrence of multidrug- and pan-resistant strains presents a serious global threat. About 87–100% of C. auris isolates are resistant to fluconazole, 8–35% to amphotericin B and 0–8% to ECH1. In contrast to other Candida species, C. auris can spread easily from person to person by direct and indirect contact. Limited treatment options, tolerance to disinfectants and heat, and the ability to colonise skin and smooth surfaces facilitate the spread of the fungus in hospitals and intensive care units. C. auris is classified as an urgent threat by the US Centers for Disease Control and Prevention and is ranked in the highest prioritization category by the World Health Organization1,2. Increasing numbers of cases and outbreaks caused by C. auris have also been reported in at least 15 European countries up to 20212,3.
Clinical picture
C. auris can colonize the urogenital tract, skin, gastrointestinal tract or respiratory tract without clinical illness. Such colonization in healthy persons does not usually require therapy. However, in patients with underlying medical conditions, the pathogen can cause serious invasive infections of the bloodstream, abdomen, ears or wounds. Moreover, nosocomial infections in vulnerable patients have relatively high mortality rates, ranging from 30% to 72%4. Typical risk factors for invasive C. auris infection include broad-spectrum antibiotic therapy, central venous catheterisation, or parenteral nutrition. In addition, C. auris infection poses a high risk for patients on ventilation in intensive care units2,5.
Laboratory identification
Laboratory identification of C. auris is important for implementing measures to oversee or limit the spread of the fungus. C. auris is difficult to identify by traditional fungal culturing, as it can be misidentified as other types of yeasts by phenotype. If certain species, for example C. haemulonii, are initially identified from isolates or if the species cannot be identified, further characterization is needed to determine if the isolate is C. auris6. Polymerase chain reaction (PCR) and matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) are the most commonly used tools for C. auris identification. Whole genome sequencing (WGS) has also been used.
PCR offers the advantage of being a culture-independent technique with a much shorter turnaround time than the other mentioned methods, yielding results within a few hours7. Real-time PCR provides the fastest test results and is less labor-intensive and easier to perform at higher throughput than conventional PCR. A suitable target for PCR-based C. auris identification is the internal transcribed spacer (ITS) gene. This provides high specificity and, due to the presence of multiple copies in many strains, also high sensitivity.
ECH resistance
ECH are the recommended frontline treatment for C. auris infection. These antifungals can treat most C. auris infections, especially those that are resistant to other agents. However, certain mutations in the HS1 regions of the FKS1 gene limit the susceptibility of C. auris to ECH. These mutations result in critical amino acid exchanges, the most common of which are S639F, S639Y and S639P8.
Real-time PCR assays
Two real-time PCR assays have been developed to address different laboratory needs in the identification of C. auris. The EURORealTime C. auris ECH-R (Euroimmun) provides identification of C. auris and determination of ECH resistance-associated mutations in one assay. The Candida auris Real-Time PCR Reagents (Revvity) with dUTP/UNG carryover prevention system provides qualitative C. auris screening. Both assays are currently available for research use*.
In both assays, the identification of C. auris is based on amplification of a partial genetic region of the multicopy ITS 1 & 2, which enables sensitive detection of C. auris. The EURORealTime assay additionally detects FKS1 HS1 mutations coding for S639F/Y/P, which serve as ECH resistance markers and additionally identify C. auris. Both assays include control primers/probes for process monitoring and/or sample quality check.
The procedures can be performed using DNA extracted, for example, from human skin swabs or laboratory cultures, and for the Candida auris Real-Time PCR Reagents also from environmental surface swabs. The semi-automated DNA extraction procedure using the chemagic™ Pathogen NA Kit H96 (Revvity) and the chemagic™ 360 instrument is recommended. Both PCR assays are compatible with various real-time PCR thermocycler systems, and results are generated in less than two hours.
Analytical evaluation
The high specificity of the primers and probes to detect all five C. auris clades and the ECH resistance markers was verified by in silico analyses against C. auris genome sequences available in public databases. No cross-reactivity with other Candida species or microorganisms that are frequently found in skin infections was predicted. The limit of detection for both assays and for both ITS and FKS1 HS1 targets amounted to 30 copies per PCR reaction using synthetic C. auris plasmid spiked into the PCR reagents. Using gDNA extracted from C. auris suspensions, detection rates of 100% were obtained at concentrations as low as 600 cfu/mL for ITS and 1800 cfu/mL for FKS1 HS19,10.
In analyses with the EURORealTime C. auris ECH-R using synthetic plasmid DNA simulating the FKS1 HS1 wildtype S639, as well as two genetic variants S639S (wild-type silent mutation) and S639T, no relevant cross-reactivity with the mutation-specific probes was found. Plasmids containing mutations coding for S639F/Y/P generated strong positive signals in the real-time PCR detection, allowing a clear distinction from the wild type. In further analyses using laboratory cultures, 23 strains of C. auris covering all five clades were successfully detected via the ITS target. One of the 23 strains contained an ECH-resistance mutation (S639F), which was correctly identified. The 22 wild-type strains tested negative for the respective mutations. Thus, mutations conferring ECH resistance are reliably determined with the EURORealTime C. auris ECH-R assay using highly specific probes without cross reactivity to wild-type strains9.
Summary
- New real-time PCR assays enable reliable identification of C. auris and of the specific echinocandin resistance markers S639F/Y/P.
- Semi-automated extraction provides simple DNA isolation.
- The assays are applicable on various real-time PCR thermocyclers.
- DNA quality is verified by detection of an endogenous control gene.
- Accurate results are obtained in less than 2 hours.
*For research use only, not for in vitro diagnostics. Regulatory status, precise intended use and product availability must be verified for the user‘s individual jurisdiction.
This guest editorial article was written by Euroimmun.
References
1. WHO fungal priority pathogens list to guide research, development and public health action. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
2. Aldejohann et al. Rise in Candida Auris Cases and First Nosocomial Transmissions in Germany. Dtsch Arztebl Int 2023; 120: 477-8. doi: 10.3238/arztebl.m2023.0047
3. Kohlenberg A. et al. Increasing number of cases and outbreaks caused by Candida auris in the EU/EEA, 2020 to 2021. Euro Surveill. 2022;27(46):pii=2200846.
4. Cortegiani et al. Epidemiology, clinical characteristics, resistance, and treatment of infections by Candida auris. J Intensive Care. 2018 Oct 29;6:69. doi: 10.1186/s40560-018-0342-4.
5. About Candida auris (C. auris). www.cdc.gov/candida-auris/about (accessed May 2024).
6. Identification of Candida auris. www.cdc.gov/candida-auris/hcp/laboratories/identification-of-c-auris.html (accessed May 2024).
7. Sekyere et al. Candida auris: A systematic review and meta-analysis of current updates on an emerging multidrug-resistant pathogen. Microbiologyopen. 2018 Aug;7(4):e00578. doi: 10.1002/mbo3.578.
8. Rybak et al. The molecular and genetic basis of antifungal resistance in the emerging fungal pathogen Candida auris. Current Opinion in Microbiology 2022, 70:102208. doi: 10.1016/j.mib.2022.102208
9. Filippis et al. New real-time PCR assay for detection of Candida auris and echinocandin resistance-associated mutations. Scientific presentation at the Association of Public Health Laboratories (APHL) Annual Conference. Milwaukee, USA, May 2024.
10. Veling et al. Rapid Candida auris Screening and Echinocandins Resistance Detection Through an Automated High-Throughput Extraction and Real-time PCR Solution. Lab Matters. Association of Public Health Laboratories (APHL) 2024 Annual Conference (in press).
