Improving organoids to advance understanding of lung development and disease
Dr. Sandra Leibel, USCD and Rady Children’s Hospital, discusses physiologically relevant lung organoids, the power of automated live-cell imaging and the search for new biotherapeutics
18 May 2021Animal models can only take you so far. No matter how much we try to humanize them by introducing specific receptors, they fall short of replicating human disease and development. And that is where organoids can be a game changer, particularly when used in conjunction with animal models. Recent advances in human lung organoid development are accelerating the search for new therapeutics to treat respiratory diseases such as COVID-19, but also enabling more physiologically relevant study of lung development and disease following premature birth.
Dr. Sandra Leibel is a developmental biologist working across both these frontiers in an academic and hospital setting in California, USA. Employed as an assistant clinical professor at the University of California, San Diego (UCSD), and also as a neonatologist at Rady Children’s Hospital and Jacobs Medical Center, she is deriving lung organoids from stem cells and using automated live-cell imaging to track and manipulate cell differentiation, as well as monitoring in real time how lung cells are being destroyed by viruses such as SARS-CoV-2.
Biopharma drug discovery using organoids
Leibel’s current work at UCSD is focused on battling COVID-19 with the use of her human lung organoid platform for testing various bioactive compounds. “We run various compounds to see which ones decrease the infectivity of lung airway cells, as well as alveolar cells,” she says. But the work goes much further than that: “We’re also able to examine different sexes of our stem cell-derived organoids to see if there’s a difference between male and female cell reactions to the various compounds.”
And animal models are not entirely redundant in this brave new world of organoids. Leibel explains: “For COVID-19 study, the intact lung system in animal models, with vasculature and immune cells, is all-important, but animals still do not replicate human disease. It remains imperative to test the bioactive compounds that maybe have a positive hit in the animal model on a human-based lung system.”
Generating such a system, or organoid, requires great skill, and making them “physiologically relevant” is even more of a technical challenge.
Physiologically relevant lung organoids
Human lung organoids can be derived from both induced pluripotent stem cells (iPSCs) and primary lung tissue. Whether they are used in the fight against COVID-19 or to better understand the significant breathing challenges faced by preterm babies, physiological relevance is of paramount importance. “Physiological relevance is being able to replicate what is happening in the body outside in a dish. That ultimately means investing human lung cells with a population of vascularized cells as well as immune cells, so that you’re actually investigating lung tissue,” says Leibel.
However, maintaining physiological relevance is no easy task. Normal lung development in vivo is supported by multiple signals from not only the lung cells themselves but also external factors which are not fully understood because this knowledge has so far been derived from mouse models. According to Leibel, the challenge is to maintain the cells so that they differentiate correctly. “If not cultured well, they’ll tend to differentiate into other types of cells that we may not want in our culture system,” Leibel explains. The key is to maintain them in 3D format: “We found that actual organoids or spheroids maintain the physiology a lot better than growing them in a monolayer.”
Knowing that things work better in 3D is one thing but following exactly how differentiation is proceeding to ensure appropriate final cell types requires cutting-edge automated live-cell imaging technology. And Sartorius’s Incucyte® Live-Cell Analysis System is Leibel’s chosen equipment.
The underpinning technology of automated live-cell imaging
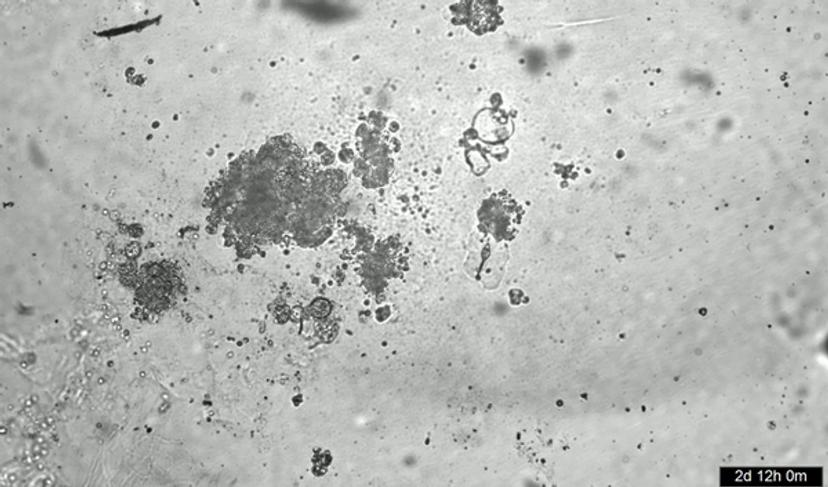
Leibel uses live-cell imaging in both her work on fetal lung development and in SARS-CoV-2 infection of lung organoids. For the former, she uses the Incucyte to study iPSC-derived lung development by using an embryonic stem cell reporter line system linked to green and red fluorescent markers. “The Incucyte allows me to grow these cells in a cultural system over a long period of time and just watch the color start to be turned on at different time points during differentiation,” says Leibel. “This allows me to tweak the various growth factors and small molecules to get the population of cells that I’m interested in, as well as learning about when they’re appearing.”
Leibel is effusive about the benefits to her work of using the Incucyte technology, which she uses to take multiple pictures of her iPSC-derived lung organoids. “This is important,” she says, “because previously, I would have to take them out once a day and manually look to see how they were developing. Now, I’m able to capture images every three to six hours and watch them closer to understand in real time what happens when I add certain growth factors.”
The ‘movie-making’ feature of the Incucyte is also a boon to Leibel, particularly in her COVID-19 work. Not only can she use it to perform staining and look at various cells within her organoids that are infected by coronavirus, but she can take footage of infected lung organoids. “I’ve been able to watch the timing of when cells actually get destroyed by the virus. That gives me a good sense of time for the actual viral replication process, but also the type of cell death that the virus induces in the lung organoids themselves,” Leibel enthuses.
Future developments
Replicating lung tissue more accurately remains a key aspiration of Leibel’s work. Her current lung organoids contain two cell populations – epithelial and mesenchymal cells. Two important cell populations are currently missing. Leibel explains, “For our future work, we’re actually differentiating macrophages and endothelial cells from pluripotent stem cells. Then we’ll tag them with markers, culture them with our existing lung organoids and use the Incucyte to watch them gather together and become a full lung tissue organoid.” She further adds, ”Finally, we’ll infect them with SARS-CoV-2 and watch how the macrophages and the endothelial cells change in response to the infection.”
Find out more about Leibel’s work at the Rady Children’s Hospital and how Sartorius’s Incucyte® Live-cell Analysis Systems could help you.
Visit the SelectScience Biopharmaceuticals Special Feature for more on the latest research, techniques and technologies advancing the field.

