New Phesi data reveals more than 100 diseases are being studied using GLP-1 therapies
Analysis shows potential for patient benefits to extend far beyond obesity, opening doors to a new era of multi-disease prevention and care
15 Sept 2025New analysis from Phesi of 583 recruiting clinical trials or trials about to start involving GLP-1 receptor antagonists finds more than 100 diseases are now being investigated in the context of GLP-1 usage. This includes trials directly evaluating GLP-1s as interventions, as well as those exploring comorbidities and modulatory effects. The analysis leverages real-world data from Phesi’s Trial Accelerator™ platform and a newly published Digital Patient Profile (DPP) of GLP-1 patients. The findings reflect growing interest in GLP-1s as a broader modulatory pathway across multiple indications including cardiovascular disease, polycystic ovary disease, osteoarthritis and multiple cancers (Table 1).
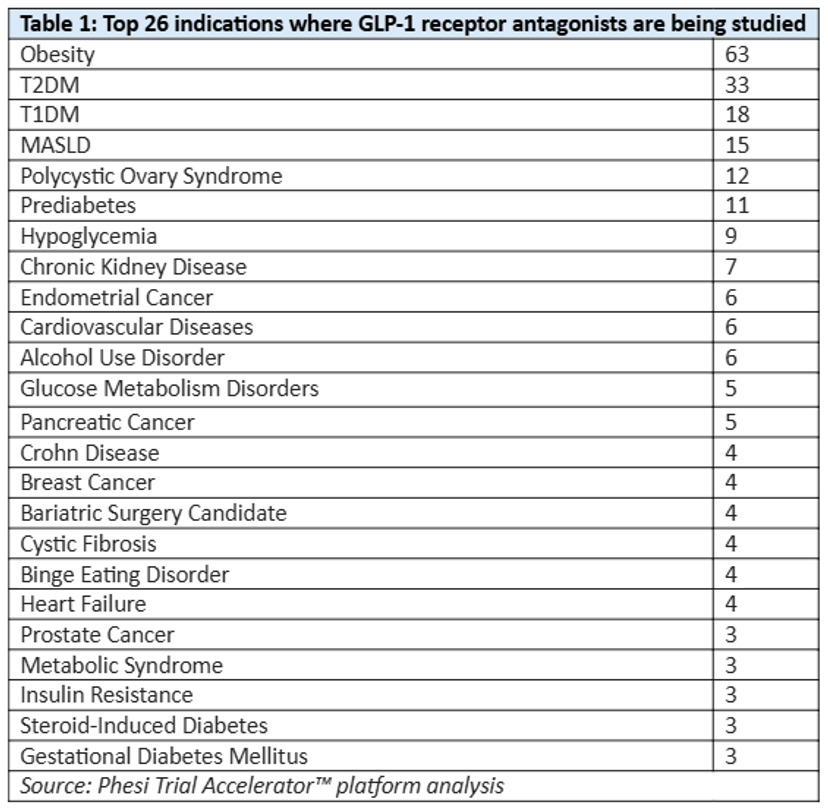
Table 1: Top 26 indications where GLP-1 receptor antagonists are being studied
“Scientific curiosity is increasingly centered on understanding how weight and metabolic factors intersect with other disease areas, including cardiovascular, inflammatory and neurological conditions,” said Dr Gen Li, Founder and President, Phesi. “The data show a clear trajectory – GLP-1s began in diabetes, moved into obesity, and now we’re seeing increasing application across a spectrum of diseases with shared risk profiles. The goal for the industry is not just treating obesity, but treating the entire constellation of conditions associated with it. GLP-1s are forcing a re-evaluation of how we define, diagnose and treat disease – prevention is emerging as the new blockbuster. With the right data, sponsors can target the right patients earlier, saving time, money and lives.”
Phesi’s analysis reveals that GLP-1 use is growing rapidly, with many patients presenting overlapping conditions, such as hypercholesterolemia and hyperlipidemia. This suggests GLP-1s are increasingly used to target systemic disease clusters rather than single indications. In some cases, GLP-1s are used adjunctively in non-obesity-related treatments (e.g. osteoarthritis), where initial findings suggest possible synergistic effects. Looking at how this uptick in activity is impacting obesity trials, Phesi finds that cycle times are increasing; the average duration of obesity trials has grown over the past two decades, with trials that used to take 10–20 months now often taking 25–45 months (Fig.1).
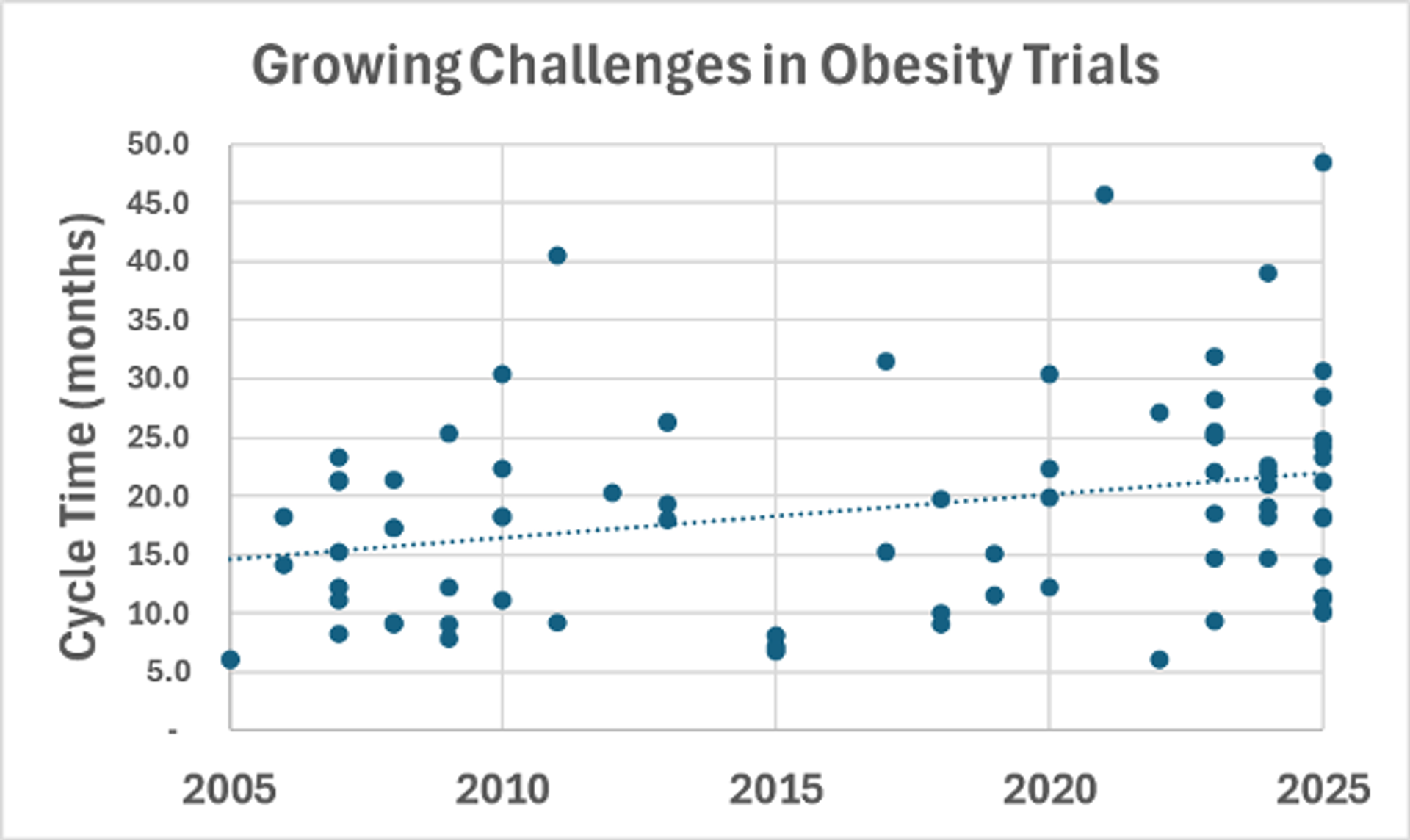
Figure 1: Trend in clinical trial cycle times for obesity-related studies between 2005 and 2025
The implications of these trends are significant for R&D, clinical trial design and healthcare strategies. GLP-1s exemplify the shift from siloed disease treatment to a holistic, patient-centered approach, where a single intervention could address multiple related conditions. Clinical specialisms will also be forced to adapt; as diseases like cardiovascular conditions, MASH and diabetes increasingly converge, physicians and trial designers must move beyond single-disease expertise to multi-indication decision-making. Operationally, clinical development organizations need to become smarter and data-driven to ensure portfolios and programmes remain viable against this evolving backdrop.
“GLP-1s have the potential to reshape how we think about disease prevention, not just treatment. And as GLP-1 usage grows, the volume of real-world data (RWD) is increasing rapidly,” said Jonathan Peachey, Chief Operating Officer, Phesi. “This may present a challenge to clinical development with competition and recruitment bottlenecks. But it also offers both an opportunity and a solution. Sophisticated clinical data analytics combining RWD and disease modelling will unlock insights that optimize clinical operations, reduce costs, drive down patient and investigator site burden, and enhance regulatory strategies. These insights will also afford sponsors and clinicians deeper understanding of longitudinal outcomes in treated patients and provide data that can be fed back into analysis. This is critical because we are at the early stages of understanding disease convergence, and hypotheses are still emerging that will require significant RWD to substantiate.”
Phesi’s DPP is created from analyzing 1,896,194 patients about to be treated by GLP-1 inhibitors from 69,652 hospitals and clinics in 81 countries in the past 20 years. The findings confirm that fasting plasma glucose concentration is correlated with HbA1c but also find no apparent correlation between BMI and HbA1c – confirming that BMI is not always an accurate measure of health. A DPP provides sponsors with a statistical view of real-world patient attributes – such as demographics, comorbidities and baseline outcomes – to support better trial design, build digital twins and identify lead enrolling investigator sites, delivering development in faster timelines and with improved data quality. Phesi’s DPP provides the crucial foundation for sponsors to make faster, smarter decisions in a fast-evolving therapeutic landscape defined by GLP-1 convergence.
