B•R•A•H•M•S Procalcitonin testing offers a smarter, cost-saving approach to sepsis management
Learn why the clinical lab plays an important role in antibiotic stewardship programs and sepsis care in this cross-departmental discussion between pharmacy, lab, and critical patient care providers
17 Sept 2025
The ability to differentiate bacterial infections from other causes of inflammation offers a game-changer. Image courtesy of Siemens Healthineers.
In the modern hospital setting, sepsis remains one of the most dangerous and costly threats to patient care. Despite advancements in diagnostics and treatment protocols, early and accurate detection of sepsis continues to challenge clinicians. At the same time, overuse of antibiotics, once considered miracle drugs, has led to antibiotic resistance, a mounting public health crisis.
Antibiotic resistance is now driven not just by overprescription in outpatient settings, but by hospital protocols that often prioritize early treatment over diagnostic precision. In the name of safety, clinicians frequently default to prescribing broad-spectrum antibiotics. But that safety net comes with a potential cost: disrupted microbiomes, increased risk of C. difficile infections, longer hospital stays, and drug-resistant infections.
B•R•A•H•M•S Procalcitonin (PCT) testing, a biomarker-based approach that helps differentiate bacterial infections from other causes of inflammation, is changing that equation.
"Sepsis is the leading cause of hospitalizations, with approximately 6% of all hospitalizations" attributed to sepsis, says Dr. Jim Aguanno, senior clinical and scientific consultant at Siemens Healthineers, during a recent P.A.C.E.®-accredited webinar hosted by SelectScience. "More than 1.7 million people in the U.S. are diagnosed with sepsis each year, one every 20 seconds."
PCT testing offers a clinical and economic lifeline. The biomarker is sensitive and specific to bacterial infections, helping clinicians answer three critical questions: Does the patient need antibiotics? Are antibiotics working? And when is it safe to stop them?
A smarter way to guide antibiotic use
The traditional approach to treating suspected sepsis often defaults to a full course of antibiotics over five, seven, or even ten days, regardless of whether the infection is confirmed. But bacterial infections do not follow a standard timeline, and neither should treatment. B•R•A•H•M•S PCT testing enables a more individualized approach.
“PCT can help us differentiate between a bacterial and a viral infection, which is very important,” explains Dr. Michael Broyles, director of medical affairs and biomarkers at Thermo Fisher Scientific. “Then, because it tells you something about the severity of bacterial burden, it also provides useful information.”
Once elevated, PCT levels typically decline by 50% every 24 hours if treatment is effectively controlling the infection. This kinetic pattern makes it possible to monitor a patient’s response to therapy in near real time. If levels are dropping appropriately and the patient is improving, antibiotics can often be discontinued earlier than traditional protocols would allow. Conversely, if PCT remains high or increases, it signals potential treatment failure or unresolved infection, prompting timely intervention. “We can use that elimination half-life to determine… are antibiotics working, and many times to determine when we can safely stop,” says Dr. Broyles. “This is very valuable for the clinician.”
Dr. Broyles points to an extensive study of more than 2,100 patients in a mature antimicrobial stewardship program, where incorporating PCT testing led to a 47% reduction in antimicrobial days of therapy. Even more striking was the clinical impact: “Hospital-caused mortalities reduced 62%, and mortality from infection was 59%,” shares Dr. Broyles.
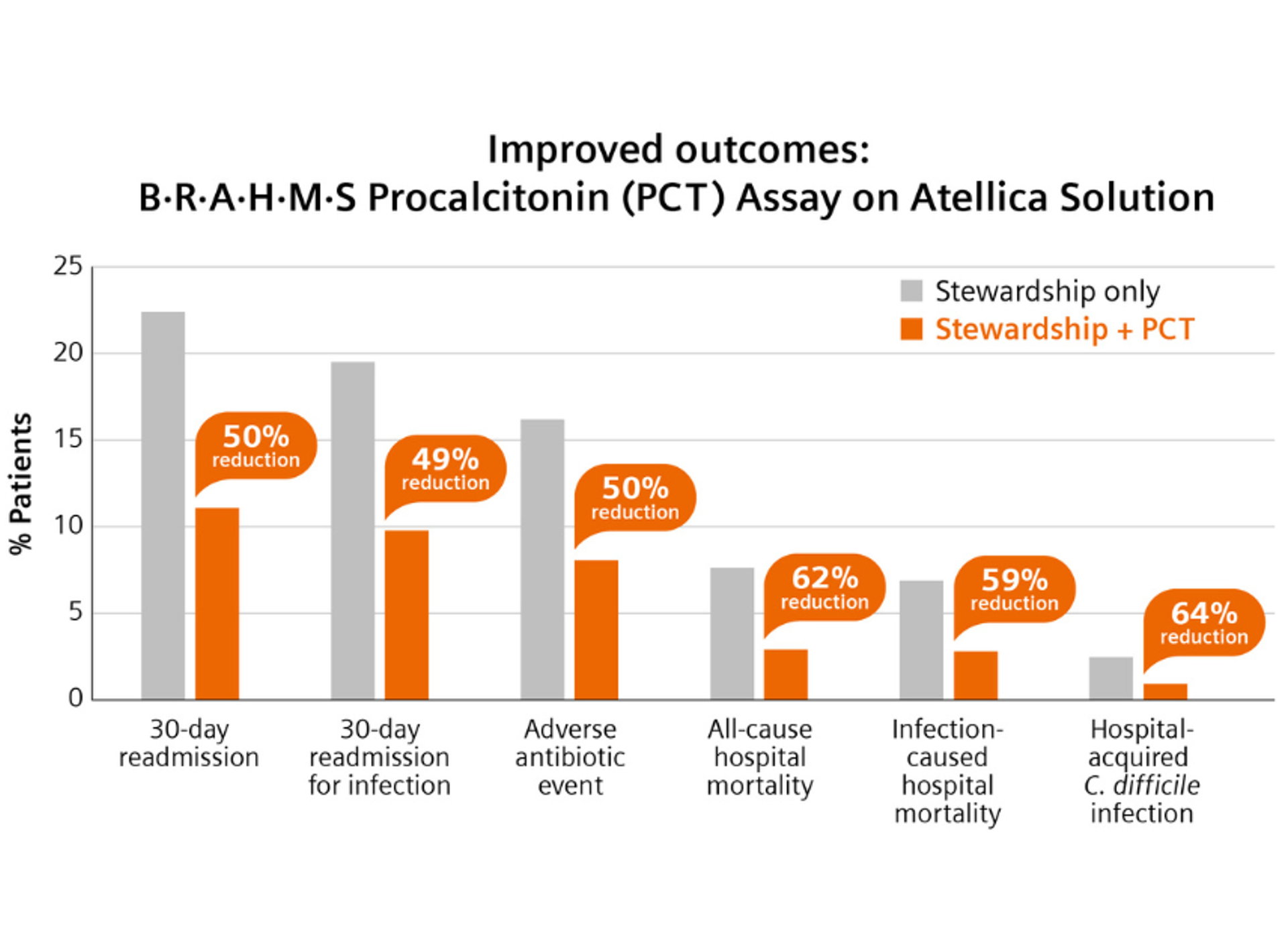
This graph details improved patient outcomes when using both antimicrobial stewardship and PCT testing compared to antimicrobial stewardship alone.
Image courtesy of Siemens Healthineers.1
Fewer ventilator days, lower readmissions
Beyond survival rates, B•R•A•H•M•S PCT testing improves ICU metrics that directly affect hospital costs. “In sepsis, there was a two-day reduction in ventilator days,” Dr. Broyles notes, referencing a U.S.-based meta-analysis of 13 studies.2 That same data shows a six-day reduction in antibiotic treatment duration.
That is more than a clinical win; it is an economic one. Patients were discharged earlier, experienced fewer complications, and avoided unnecessary exposure to medications.
The benefits extended to readmissions, too. “Clinicians always say, ‘Well, if I give you fewer antibiotics, my patients are going to come back” says Dr. Broyles. “If you give antibiotics to the right people for the right duration, they don’t come back.”
Preventing C. difficile and saving on ICU costs
Antibiotic overuse is a known trigger for Clostridioides difficile infections, which can be debilitating, deadly, and extremely costly to treat. With B•R•A•H•M•S PCT guidance, unnecessary antibiotic exposure goes down, and so does C. diff incidence.
“We know that C. diff is typically a reaction to overuse of antibiotics,” says Dr. Eric Gluck, director of critical care services at Swedish Covenant Hospital. “Patients in the intensive care unit where B•R•A•H•M•S procalcitonin is used as a biomarker are going to receive less antibiotics... and those two things will result in a lower incidence of C. diff.”
In one implementation,1 hospitals saw a 64% reduction in C. diff infections. Reduced antibiotic exposure also led to fewer adverse events and complications, key drivers of extended ICU stays and higher insurance claims.
Differentiating heart failure and sepsis
PCT can also help clinicians distinguish between lookalike presentations, such as heart failure and pneumonia, a diagnostic dilemma with high stakes.
Dr. Gluck described two ICU patients who arrived just hours apart, both with respiratory distress and bilateral infiltrates. “It was indistinguishable until we started doing more sensitive evaluations,” he says.
The first patient had elevated lactate but low PCT, ultimately pointing to heart failure. The second showed a rising PCT level the next day, confirming bacterial pneumonia and justifying antibiotic therapy. “So for these two patients, who looked virtually identical on presentation, we can identify that the first patient was in heart failure. The second patient was septic,” Dr. Gluck explains.
From lab cost to hospital-wide value
For laboratorians and hospital administrators, upfront costs are a valid concern. Effective PCT testing requires stat availability and round-the-clock access. But experts argue that the investment is offset many times over in downstream savings.
“Yes, the laboratory could take a hit, but with the savings in ICU days, antibiotics, and the rest… there’s a significant savings possible,” says Dr. Aguanno. “The whole point of this is it is a great opportunity for the laboratory and the lab director to get out of the silo… and talk to their clinical colleagues.”
Cross-department collaboration is essential. In successful implementations, ICU clinicians, pharmacists, emergency physicians, and lab directors come together with a shared goal: optimizing antibiotic usage without compromising care.
“It does take a broad group of people to really get this test implemented properly,” says Dr. Aguanno.
What makes B•R•A•H•M•S PCT stand out is its combination of clinical utility and operational impact. It gives clinicians timely, actionable data. It helps labs move from cost centers to value drivers. And it allows hospitals to care for patients more effectively without relying on blunt one-size-fits-all protocols.

Watch the on-demand webinar to hear more from Dr. Eric Gluck, director of critical care services at Swedish Covenant Hospital, Dr. Jim Aguanno, senior clinical and scientific consultant at Siemens Healthineers, and Dr. Michael Broyles, director of medical affairs and biomarkers at Thermo Fisher Scientific.
To learn more about this, watch the P.A.C.E.®-accredited webinar on demand.
All trademarks are the property of their respective owners.
References:
1) Broyles MR. Open Forum Infect Dis 2017;4:10.1093/ofid/ofx213. DOI: 10.1093/ofid/ofx213
2) J.C. Mewes, et al. The cost impact of PCT-guided antibiotic stewardship versus usual care for hospitalised patients with suspected sepsis or lower respiratory tract infections in the US: A health economic model analysis. April 2019. DOI: 10.1371/journal.pone.0214222
