Single-cell analysis technology: A gateway to early metastatic cancer detection
Learn how innovative technologies are optimizing CTC (circulating tumor cell)-based liquid biopsies to improve cancer diagnostics.
6 Dec 2021
In the age of non-invasive procedures, liquid biopsy analysis has transformed cancer diagnostics and how clinicians design chemotherapeutic protocols for their patients. Here, SelectScience® speak with viral pathologist Dr. Bruce Patterson, who provides insight into how his team at IncellDx are pioneering cell analysis workflows to develop better blood-based cancer diagnostics at the frontier of precision medicine.
CTCs and the link to early cancer detection
Historically, tumor detection and diagnostics have heavily relied on invasive techniques, such as tumor biopsy or fine needle aspiration. These would focus on analyzing the primary tumor, i.e., the tumor at the site of its origin. To study tumor progression and the response to therapy, these techniques would be repeated over the course of the disease. The results would then inform the clinicians on how to optimize the course of therapy for their patients.
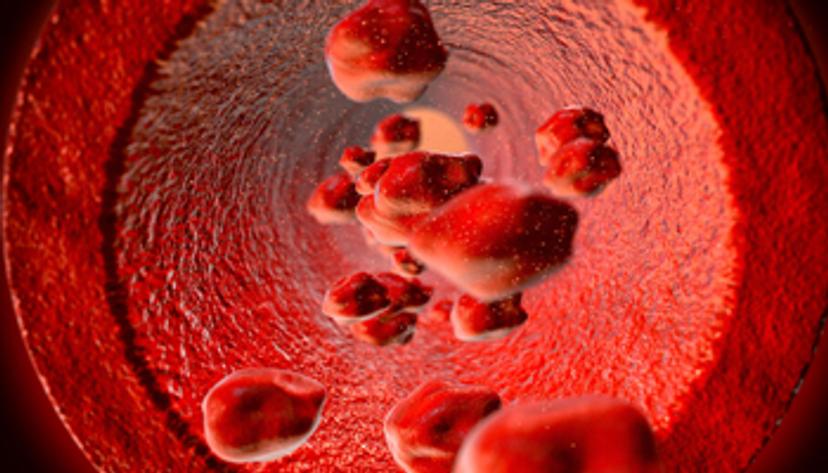
This has changed dramatically today in our age of ‘non-invasiveness’, says Dr. Bruce Patterson, CEO & Founder at IncellDx, a diagnostic company focusing on precision medicine. “Today, clinicians rely on non-invasive techniques such as liquid biopsy, which use a routine blood sample to analyze the different characteristics of a tumor. Liquid biopsy centers on two main ways of detecting and monitoring cancer via a blood draw, either by tracing cell-free genetic material (DNA or RNA), or by capturing and analyzing tumor cells circulating in the blood (known as CTCs),” he explains.
While both the analysis types in liquid biopsy are non-invasive, focusing on cell-free genetic material may not account for the heterogeneity of the tumor. This method only provides limited contextual information on its origin. However, capturing information from CTCs mitigates this risk to a great extent. It provides insight into the cell types, the mutations, and the characteristics of the tumor that is potentially metastasizing. This is not to say there are no genetic or protein differences between the cells from the peripheral blood and those that make-up the primary tumor; only that such differences do not necessarily interfere with cancer diagnosis. “Ultimately, it is the metastasis - caused by the CTCs - that turns fatal in a patient with cancer, and not always the primary tumor. Studying CTCs is a gateway into early metastasis detection. It also enables the design of a chemotherapeutic protocol that treats the metastasis alongside targeting the primary tumor,” elaborates Patterson.
In analyzing liquid biopsy samples, the limiting factor is always the sensitivity of the platform being used, regardless of whether it is based on cell-free material, CTCs or even exosomes. The very first CTC instruments had poor sensitivity, requiring many cells and repeated sample collection for an insightful analysis from a single patient. Today, the goal is to capture sufficient CTCs in one step and do multiple types of analyses on the cells, at minimal inconvenience to the patient. “This is where the Celselect™ Slide technology from Bio-Rad proved optimal for single-cell isolation of CTCs, as opposed to some of the other technologies that we tested previously,” asserts Patterson. The IncellDx team uses the Celselect™ Slides with the Bio-Rad Genesis isolation system, which provides users with analytical control to optimize protocols and customize antibodies.
An optimized CTC isolation workflow
Patterson highlights the Genesis system’s sensitivity, flexibility, and ease-of-use as the primary reasons why the IncellDx-Bio-Rad pairing works well for his team’s research. Moreover, on the logistical side, the compact size of the Genesis system is a significant advantage when it comes to using laboratory workspace efficiently.
In fact, by leveraging the Genesis System by Bio-Rad, the IncellDx team has built one of the most analytically sensitive workflows on the market. “We start with blood sample collection through Streck’s optimized blood-collection tubes, which stabilizes the CTCs. We then use the IncellDx’s BioINK kit, which utilizes a preservative that does not crosslink or damage any of the proteins,” says Patterson. “This prepared sample is run through the Celselect™ Slide, which utilizes microfluidics to isolate and capture enriched CTCs. The output cells can either be labeled with antibodies using immunocytochemistry techniques or recovered for further analysis such as next-generation sequencing (NGS).” The IncellDx team’s workflow is designed recover 90% of tumor cells grown in culture, with a promised upside of at least 20% over other workflows available in the market. With the unique approach of combining the strengths of the Streck tube, the IncellDx BioINK kit, and the Bio-Rad Genesis System, the protocol provides an output optimized for NGS analysis.
Biomarker-enabled prediction of CTCs
The InCellDx team recently published their findings on CTCs in a hallmark lung-cancer paper in the journal of Translational Oncology.1 The paper highlights findings from a protocol that provides reproducible analytical sensitivity down to five CTCs in a 4-milliliter sample of blood. The work detailed in the paper utilizes extensive bioinformatics with 20-color detection by flow cytometry to show that non-small cell lung cancer tumors have a signature that can predict if the patient has CTCs in their blood.
Providing an insight into the details of the work, Patterson explains, “When your body recognizes a tumor, it triggers an immune response, and regulatory T cells (Treg) enter the site to fight the tumor. However, the Treg cells also trigger a cascade of processes that begin to shut off the body’s immune response to prevent autoimmunity, as the body recognizes the cancer cells as its own. This results in a ‘lack of immune control’, allowing tumor cells to escape into the blood, giving rise to the CTCs, and ultimately leading to metastasis. Our work identifies a variety of checkpoint markers (including CD103 and CCR5) on the Treg cells that trigger the shut-off of the immune response and connects the markers to the presence of CTCs in the patient. By studying these markers, we can not only predict the presence of CTCs, but we can also design immuno-oncology therapies inhibiting the mechanism the shuts off the immune system’s anti-tumor response.”
The future of early cancer diagnostics
The findings from InCellDx’s Translational Oncology article have a direct implication in enabling early detection of potential metastasis, along with aiding the early characterization of cells that are metastasizing. By explaining the underlying mechanism that leads to CTCs, these findings also lay the groundwork for the clinical world to devise multi-drug treatment strategies for long-lasting response in patients with cancer.
Patterson hopes that early detection through non-invasive liquid biopsy methods will be incorporated in a routine manner in clinical practice worldwide, which he believes is the way forward in cancer management. “At IncellDx, we are, and we will continue to contribute to advancing early cancer diagnostics, which we hope will help in making many cancers manageable and curable”, Patterson concludes positively.
References:
Wang X, Jaimes M, Gu H, et al. Cell by cell immuno- and cancer marker profiling of non-small cell lung cancer tissue: Checkpoint marker expression on CD103+, CD4+ T-cells predicts circulating tumor cells. Transl Oncol. 2021;14(1):100953. doi:10.1016/j.tranon.2020.100953

