The Mobile Laboratory: How a Scientist Tests for Infectious Diseases out of a Suitcase
Read how Dr. Ahmed Abd El Wahed created a mobile laboratory to keep his research going even in corners of the world with poor infrastructure
22 Aug 2017
As an infectious disease researcher, Dr. Ahmed Abd El Wahed does not always work within the boundaries of his laboratory or even his country. His research travels with him in a mobile laboratory, as he works at the center of epidemics like Ebola and Zika outbreaks.
DNA amplification, an important step in infection diagnosis, although very commonplace in life sciences, is particularly challenging while in the field. You must be familiar with routine DNA amplification using PCR with extreme temperatures: a high denaturing temperature, a medium annealing temperature and finally a cool 4°C for the final hold, before starting your reaction and letting it go for hours, at times, overnight. Such a time-consuming protocol can impede the urgency of global health concerns during a threatening infection. And the need for niche equipment, such as the thermocycler, is not feasible for a mobile laboratory.
For instance, to establish whether or not a patient tests positive for the Ebola virus at a remote location in Guinea, without access to lab facilities — all while there is immense pressure for quick answers during an outbreak — Dr. Abd El Wahed devised protocols using a new DNA amplification technology called Recombinase Polymerase Amplification (RPA).
The brainchild of TwistDx, RPA works isothermally i.e. it performs DNA amplification at a single temperature, is much quicker than PCR, with amplification data being detectable in 3-10 minutes, and occupies a position of prestige inside Dr. Abd El Wahed’s mobile laboratory.
The head of the virology laboratory, Division of Microbiology and Animal Hygiene at the University of Goettingen, Germany, Dr. Abd El Wahed discusses the origin of the mobile laboratory with SelectScience and chronicles his research across international field trips.

SS: When and how did you get the idea for a mobile laboratory?
AAEW: Along with Dr. Weidmann and Prof. Hufert, I conduct field trials to establish molecular assays for rapid detection of emerging viruses. During a typical field trip, we used to take our equipment in a box and then set up our laboratory after we arrived at the field. In 2014, I had an idea — we needed something very simple, such that anybody, even with little training, would be able to detect viral infections. My vision was three simple steps: open a box, do the test, close the box, and move on to another spot.
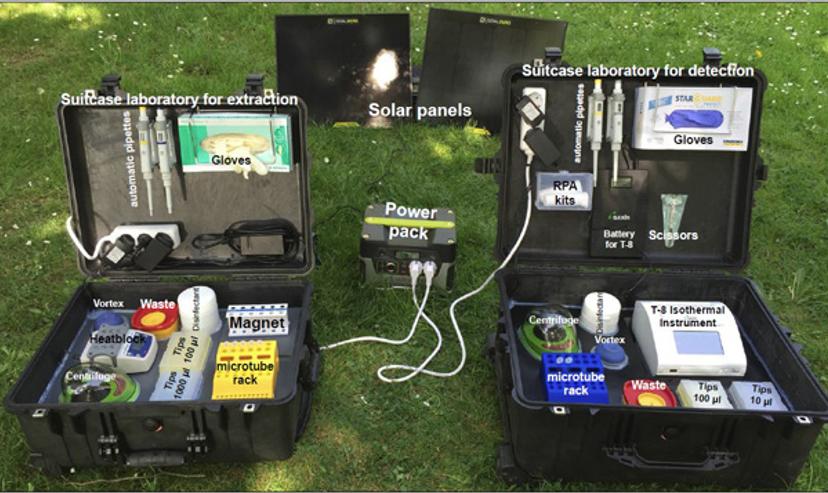
With that vision, two mobile laboratories were developed. One suitcase lab was built to host reagents and equipment to perform magnetic beads-based nucleic acid extraction; and another one was used to perform RPA, an isothermal nucleic acid amplification, and detection. The idea was to use a water- and dust-resistant suitcase that would not only be easy to transport and store reagents, but also easy to perform tests directly in it.
SS: Describe your mobile laboratory.
AAEW: We used a case equipped with a trolley measuring 56 X 45.5 cm and 26.5 cm tall, and then stuffed the bottom of the suitcase with foam cubes to absorb shocks. On top of the foam, we fixed a PVC layer. This PVC layer contained cutouts to host specific equipment.
The mobile set up is powered by solar panels and a power pack. The fully charged battery can power two suitcase labs for up to 18 hours.
SS: How have recent advances in science helped create the mobile laboratory?
AAEW: The idea of the suitcase laboratory was never possible without the RPA technology by TwistDx. In my experience, all RPA reagents are stable at 40°C for up to three months. RPA is very fast — in a maximum of 15 minutes, you can get results. Since 2012, we have been collaborating with TwistDx in many joint projects. For example, from 2014–2016, we had a collaboration project to establish a simple protocol for Ebola virus detection in the Ebola treatment centers in Guinea together with Institute Pasteur de Dakar. This was one of the best examples of how academia and companies can come together to help people.
SS: Where has your mobile laboratory travelled? And on what projects?
AAEW: To Senegal and Thailand for chikungunya and dengue field trials; to Brazil for Zika virus detection; to Bangladesh and Sri Lanka for Leishmania infections; to Guinea for the Ebola outbreak, and to Egypt for foot-and-mouth disease, H5N1 avian influenza and lumpy skin disease trials.
SS: What are the benefits of scientific resources reaching patients on site, instead of the conventional practice of patient samples being brought back to lab?
AAEW: Currently, laboratory diagnosis mostly depends on the detection of viral pathogen nucleic acid by real-time polymerase chain reaction (PCR). Since real-time PCR assays are not suitable for on-site screening, samples collected from local hospitals, autopsies, or at the site of an outbreak need to be sent to laboratories over long distances for testing. In developing countries, the necessary equipment for diagnosis is only available in a few central laboratories, with poor accessibility and limited capacity to test large numbers of incoming samples. Moreover, transport conditions of samples are inadequate and therefore lead to unreliable results. Thus, portable, accurate, simple, and rapid tests are needed to detect the pathogen at the point-of-need. In other words, a technology to help identify the outbreak as early as possible.

SS: What do you see for the future of your mobile laboratory? How do you see it evolving?
AAEW: The mobile suitcase laboratory is like the iPad, something in between a point-of-care (such as a blood sugar test) and a real laboratory (such as a real-time PCR system or rapid antigen test). I prefer to call it point-of-need. It is something we need to implement at country borders, ports of entry and low-resource settings in order to identify epidemic outbreaks as early as possible. In addition, it can be implemented in rural areas for routine diagnosis to avoid expensive building facilities.

