Tumor-specific 3D cell culture models for accurate testing of anticancer agents
Watch this on-demand webinar to discover how tissue-specific 3D culture platforms can be used throughout the drug development workflow
17 Jun 2021

The high rates of failure of new anticancer drugs in clinical trials highlight that the standard cell culture models used in drug development today do not faithfully reproduce human biology, and thus, do not accurately represent disease processes. In this webinar, Dr. Julia Kirshner, Founder & CEO of zPREDICTA, discussed the advantages of a 3D culture approach over the traditional methods, with particular emphasis on the importance of the tumor microenvironment and tissue-relevant extracellular matrix (ECM) in obtaining accurate drug response data.
In this on-demand webinar, Kirshner demonstrates how the tumor-specific microenvironment, including cellular and extracellular elements such as ECM and stroma, affects response to treatment. Kirshner also includes examples of the current use of tumor-specific 3D culture models for efficacy screening of anticancer compounds, including immuno-oncology agents, evaluation of mechanisms of drug resistance, the rescue of failed drug candidates, assessment of off-target toxicity, and multiple other applications enabling accurate evaluation of therapeutic agents throughout the drug development pipeline.
Watch on demandRead on for highlights from the live Q&A session or register to watch the webinar at a time that suits you.
Q: How can I develop 3D cancer cell culture models from primary cell culture?
JK: We make our models by creating the extracellular matrix (ECM) and the soluble environment to match the tissue and disease of interest. If we were looking at liver cancer, we would create the extracellular matrix specifically to match the liver tissue, and more specifically, the ECM of liver tumors.
There is usually a difference between a non-malignant and a malignant ECM composition. We formulate the ECM to match the state of the tissue, and then we create medium supplements that match the disease of interest. If we're looking at small-cell lung cancer versus non-small-cell lung cancer, the cytokine profiles of these patient groups will be different, so our medium supplements are different.
Then you just take primary cells from that tumor you're interested in and optimize a number of other criteria to get all cell types to propagate and everything maintains the same heterogeneity as what's seen in the tissue.
Q: For high-throughput screening of treatments on these 3D cancer cell models, how do you normalize the number of cells per well?
JK: We always start with a known number of cells per well when using cell lines, or dissociated tumor cells, or any type of co-culture system where we're mixing tumor cells and stroma cells, so we can normalize from there. From complex co-cultures or primary cell cultures where we have a truly heterogeneous population of cells, again, we know the starting number of cells.
For the truly heterogeneous populations, we have to utilize full cytometry to better understand what's happening within the culture because CellTiter-Glo® will not be the best readout to use in those situations.
When doing cultures with tissue explants, normalization there is a bit trickier as the size and composition vary. Usually, that is done by imaging or immunohistochemistry, then we can normalize the number of nuclei, and measure the cellular content that way.
Q: Why do you wait a few days before adding the treatment to your culture systems, and can you add the drugs on the same day of culture setup?
JK: You can add the drugs on the same day. However, there are reasons behind plating the cells and then waiting. We want to give cells a chance to rest and acclimate to their new environment.
If these are primary cells, they were either cryopreserved so they have to come out of thaw, or if it's fresh, there is always processing of the cells. They've been stressed already, so they're going to be hypersensitive to any kind of treatment that is applied. Therefore, the results will be skewed because the cells are going to be more responsive than they otherwise would be. We let the cells rest so that the response is not over-emphasized by this stress.
The other reason is giving cells a few days gives them a chance to start forming and organizing into the tissue-like architecture. When the drugs are applied, you see the tissue as close as possible to what would be seen in a person.
Q: Can you evaluate the effect of treatment on both tumor and stroma in your co-culture methods?
JK: Yes, we can evaluate both tumor and stroma in these cultures. We can look at pre-labeled cells and identify different cell types and look at morphology. Tumor cells usually form steroids while stroma cells form more of a spindle-shaped monolayer. By imaging, we can identify the two separate populations. We can also do flow cytometry and identify all these populations based on surface markers. It's not only epithelial versus stroma populations, but we can also look at any kind of cell type present in the culture.
Q: Can we use this cell model with substances other than drugs such as endocrine-disrupting substances?
JK: We worked with several different entities, from any kind of small molecule. We've used antibodies, we've worked with cellular, anti-cellular therapies. In terms of the reagents penetrating through the ECM, we haven't seen any issues, from small molecules all the way to antibody-drug conjugates (ADCs), or even cells. Looking at different types of compounds and different types of reagents, the system would have to be optimized for the expression of the target so that the entity will meet the cells. So far, we haven't seen any issues with actually getting the interactions within the ECM.
Q: How did you optimize r-Bone and r-Lung composition? What approaches did you use, and is there any technological space for further customized optimization?
JK: The general principle behind the development of all our systems is really understanding the tissue and the composition of the extracellular matrix of each individual tissue, and then it's optimized based on that. As the names allude to, reconstructed bone model and reconstructed lung model, each of those will have the extracellular matrix composition mimicking the organs. There would be different components in the bone versus lungs.
There is room for customization, we can make matrices differ and add additional components. Although, we try to keep things consistent within a particular tissue type so that when we're comparing patient to patient or cell line to cell line, there isn’t much variability.
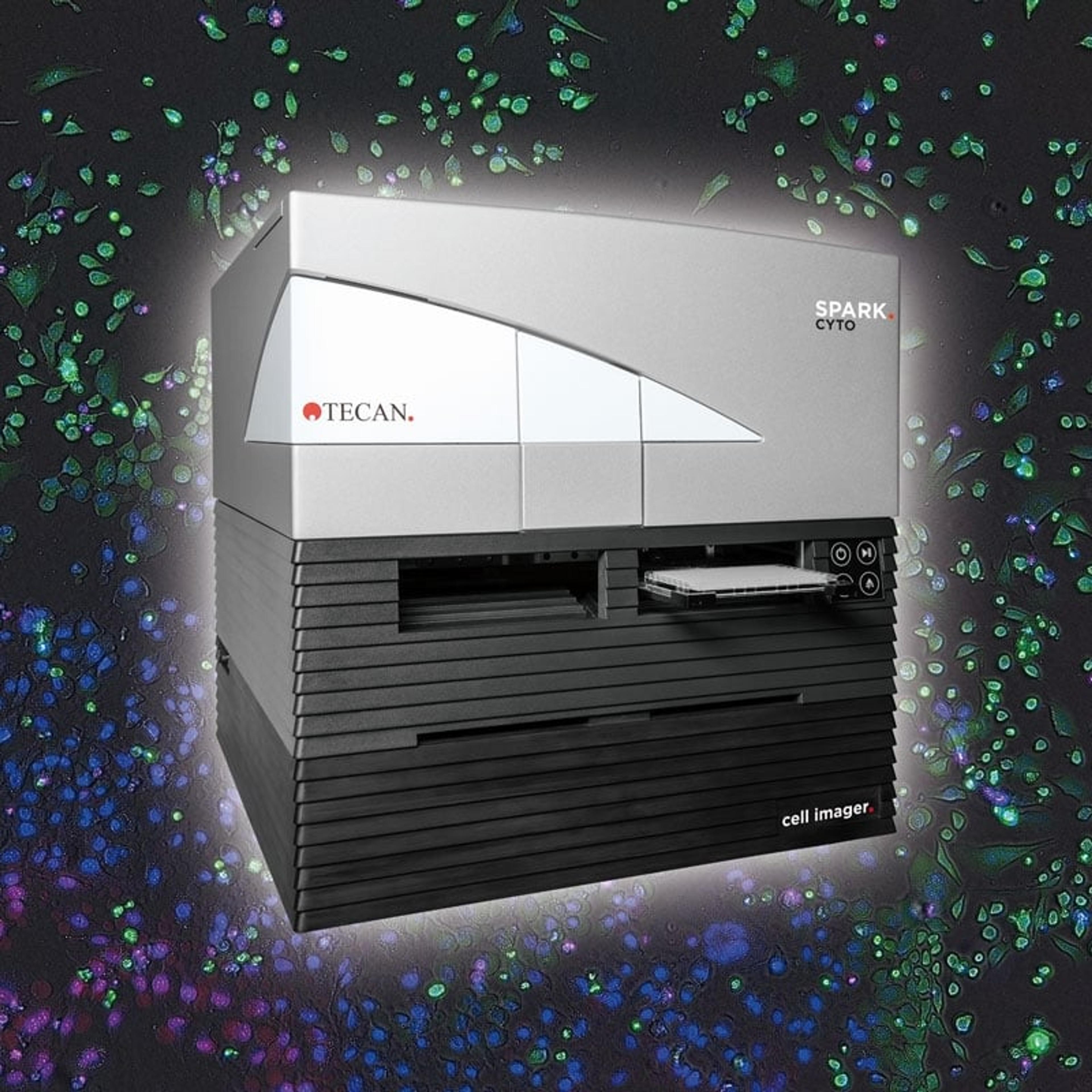
Q: Is the Spark® Cyto also able to analyze the confluency of brightfield and fluorescent images, or is it only possible to export the images and then perform the analysis in a different program?
JK: Yes, the Spark® Cyto can do confluency. You don't have to export and do it in a different program. If you want to do it in 3D cultures, we usually take images at different offsets so that we capture multiple different planes within the culture since these are all fairly thick matrices. This way, we can get a representation of what's happening. Essentially, it's like taking a Z-stack on a microscope, we know what's happening from top to bottom of the well.