Ultra-sensitive NGS-based sequencing targets mosaic disease
Leveraging duplex NGS with automated library prep, researchers move closer to developing liquid biopsy tests for rare genetic disorders
4 Sept 2024

Dr. Denny Schanze, Head of Laboratory at the Institute for Human Genetics, Otto-von-Guericke University Magdeburg
Dr. Denny Schanze, Head of the Molecular Genetic Laboratory at the Institute for Human Genetics, Otto-von-Guericke University Magdeburg, discusses his research into rare mosaic diseases, and highlights how his team is combining advanced NGS strategies with Agilent's automated library preparation technology to develop custom sequencing assays using liquid biopsy samples. Findings from this research were also presented at the European Human Genetics Conference (EHGC) in Berlin, which took place from June 1 to 4.
Unraveling the genetic culprits of mosaic disease
Dr. Schanze has spent over a decade studying genetic disorders, including rare monogenic and complex diseases. He leads the molecular genetic laboratory at Magdeburg, where his team is employing a range of NGS strategies to determine the mutations underpinning various diseases, with particular emphasis on mosaic vascular disorders.
Mosaic vascular disorders are a group of rare genetic conditions characterized by abnormal growth or development of blood vessels and surrounding tissues in a localized or segmental pattern. “One example are venous malformations,” begins Schanze. “These mainly occur in the early stages of childhood, and while some have only few impairments, others don’t stop growing – even after surgery - or led to thrombosis or embolisms.”
“We are focusing on these diseases because we know that they are caused by genetic variants but at a very low level of variant allele frequency in tissue specimens that can be obtained for genetic testing,” he continues. “Unlike somatic variants in cancer where driver mutations usually have variant allele frequencies of 20% or more, those are below 5%, 1%, sometimes even 0.5%. This means we need a highly sensitive but also specific method to study and identify these variants.”
Applying NGS for low-frequency variant detection
Mosaic disorders are caused by mutational events that arise during early embryonic or fetal development, known as postzygotic mutations. Clinical diagnosis of some mosaic disorders poses challenges due to their phenotypic heterogeneity and often incomplete syndromic features, which may even go unnoticed. Genetic diagnosis – involving the detection of disease-causing mutations – is therefore the preferred approach.
NGS offers a reliable method for diagnosing and quantifying even low-level mosaicism and can be performed on DNA from various sources, including blood, fibroblasts, urine sediment, and tissue biopsies. It is not, however, without its challenges.
When Schanze and his team first set out to employ NGS to detect mosaic disease causing variants, they focused on a small panel, around 45kb in size. They further reduced the panel size and focused on hotspot mutations in combination with unique molecular identifier (UMI) technology with large raw coverage to account for sequencing errors.
While this technique proved to be highly sensitive– even for a variant allele frequency of 0.5% – it also detects false positives due to PCR artifacts.
“We therefore changed our strategy to duplex sequencing,” explains Schanze, adding that they employed the SureSelect XT HS2 DNA Reagent Kit from Agilent to double-barcode the library, which helped remove false positives.
“We reduced our panel to only 100 targets and hotspots, so it was very focused,” he adds. “We weren't able to look beyond known hotspot targets to discover new variants, but it was very sensitive and specific, and we made many findings that could help patients.”
"More recently, we upgraded our sequencing technology, and therefore decided to increase the panel size,” he continues. “So, now we’re not only able to put the hotspots of diagnostic genes on the panel but also the whole coding sequence of the genes, and to detect new variants in these genes, besides hotspots.”
Accelerating library prep using the Magnis
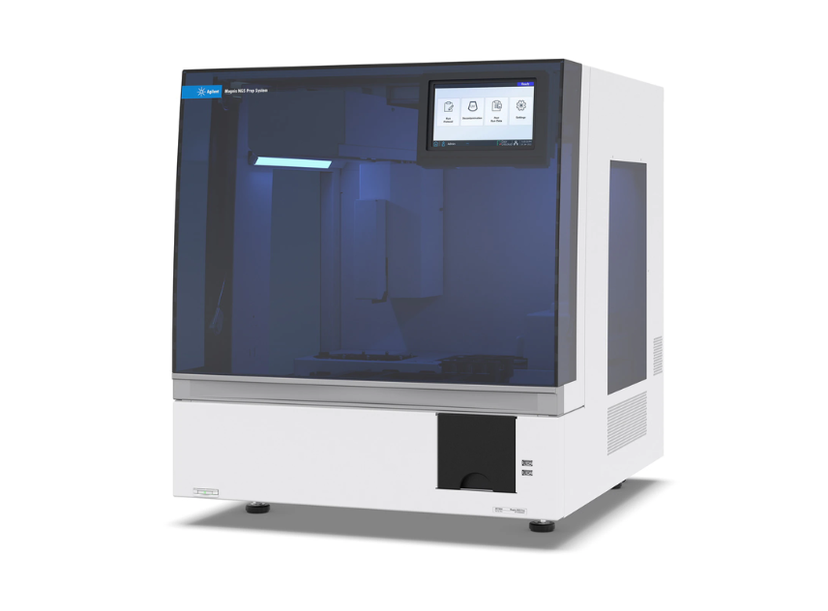
The benchtop MagnisDx system* provides a fully automated workflow for NGS library preparation. Researchers can start from total RNA with integrated cDNA conversion or unfragmented DNA with onboard enzymatic fragmentation for increased workflow efficiency.
*For In Vitro Diagnostic Use
For Schanze’s research, as with any work employing NGS, library preparation is crucial, as it directly impacts the quality and accuracy of the sequencing data obtained. To this end, his team is using the Magnis* instrument from Agilent for automated library preparation, which they have found to greatly expedite their NGS workflows. “The Magnis is a really nice instrument that saves our technicians a lot of time,” says Schanze, adding that whereas researchers typically spend several days preparing libraries manually in the lab, the Magnis allows libraries to be ready overnight.
“By the next morning, the library is ready, and we can assess the quality and load the sequences,” he continues. “Having high-quality homogeneous library prep earlier means we can get to the results faster, and this can potentially impact treatment decisions that are important for patients.”
The promise of liquid biopsies
In addition to library prep, high-quality input material is crucial to accurately detect low-frequency variants. Here, Schanze and his team are focusing also on liquid biopsies, using circulating free DNA (cfDNA) from plasma (or lymphatic fluid).
“This is a low input material – normally we get just 1 to 5 nanograms – but it’s high quality, and better than FFPE, in my experience,” he says. “The analysis of cfDNA could facilitate disease diagnosis without the need of invasive tissue sampling for patients and even help stratify patients who will benefit from targeted therapies.”
Despite the promise of NGS-based liquid biopsy tests, their clinical adoption requires thorough analytical validation, which in turn relies on the availability of well-defined reference materials. “It's hard to find good controls,” Schanze exclaims, noting that in the past commercial cfDNA reference produce noise during the analysis, because they are artificially produced to achieve cfDNA-like features and therefor are not native cfDNA. The quality of more current commercial cfDNA reference is much better and crucial for the evaluation of new tests.
However, with increasing evidence on the clinical utility of liquid biopsy diagnosis for mosaic disease, Schanze is in no doubt that such tests will eventually become implemented into routine diagnostics. “Ultimately, liquid biopsy is much easier to get from a patient if there is no surgery, and I think it will become more and more important,” he says. “There's a lot to do in the next few years – I’m aware of that, and I’m happy to be a part of it.”
The European Human Genetics Conference
Schanze presented his latest research at the European Human Genetics Conference (EHGC) in Berlin, Germany. One of his goals at this event was to highlight the potential for treating mosaic diseases, particularly those involving the Ras-MAPK and the PI3K-AKT-mTOR pathways, by repurposing existing medications once the underlying genetic causes are identified. Also discussed at the event, was the ongoing evolution of sequencing technology, as Schanze stressed the need for continuous improvement in coverage, sensitivity, and specificity. “We are still not at the end,” he states. “We have to improve this whole process more and more. We have to push the boundaries, reduce the limit of detection, and get a more inside view.”
“Ultimately, this will benefit patients by getting to the point where we can accurately diagnose and eventually treat these rare diseases,” he concludes.
*The Agilent Magnis NGS Prep system is for research use only. Not for use in diagnostic procedures.
