Using next-generation sequencing to detect Omicron and other variants
Experts at Thermo Fisher Scientific and MAKO Medical explain how NGS offers new hope in combating COVID-19 by effectively identifying and tracking existing and future variants
8 Feb 2022
In November 2021, the World Health Organization designated Omicron a “variant of concern”. Since then, the world has been placed on high alert. Omicron was first discovered in South Africa, triggering world leaders to reinstate tighter restrictions and travel bans in the hope to protect citizens from the outbreak. Omicron has been proven to be a highly transmissible variant and is suspected to be less susceptible to vaccines. This variant has multiple mutations (~50), with many located on the spike protein, which is involved in virus transmissibility and recognition of the virus by antibodies.
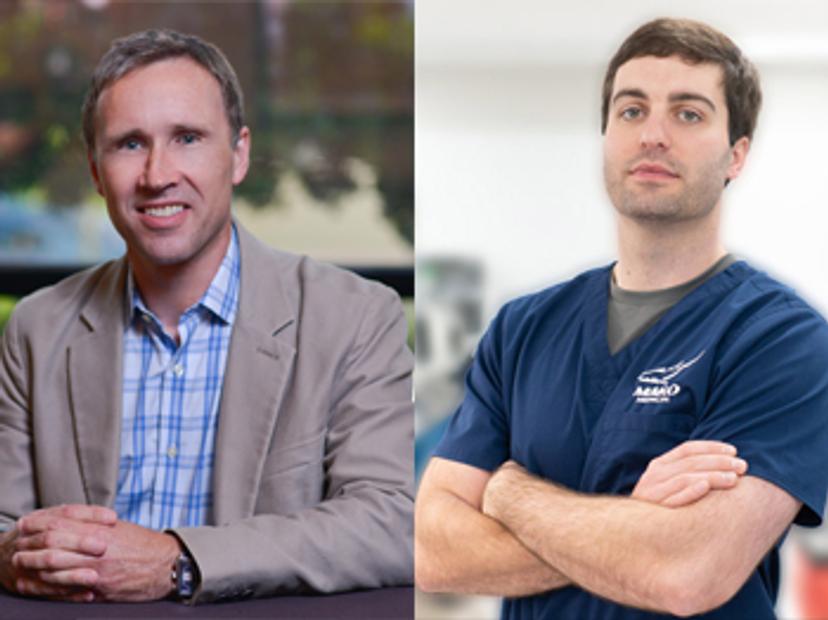
In this exclusive interview, we speak with Josh Arant, chief operating officer at MAKO Medical Laboratories, and Andy Felton, vice president, research and applied markets, clinical sequencing, Thermo Fisher Scientific, to find out more about how their organizations are tackling the global pandemic. Arant and Felton discuss the increased need for next-generation sequencing (NGS) to track and monitor the virus, and outline why NGS has become an essential tool for the rapid detection of Omicron and other potential future strains.
SS: Tell us a bit about your roles
JA: MAKO Medical Laboratories is a full-service reference laboratory headquartered in Raleigh, North Carolina. My role is to ensure the company operates efficiently and effectively, and to provide reliable and accurate results to our patients and providers.
AF: I'm the vice president of the research platform and applied markets team for clinical sequencing at Thermo Fisher Scientific. We are responsible for our next-generation sequencing solutions, including NGS-based COVID-19 surveillance.
SS: How is your company helping to tackle the pandemic?
JA: In April 2020, we brought on a COVID-19 PCR assay utilizing the Thermo Fisher TaqPath assay. At that time, we were processing COVID-19 samples for our current clientele, then the demand increased across the country and state and local governments needed testing. We increased our testing capacity and eventually got to a point where we had the capacity to run approximately 150,000 COVID-19 tests per day. In early 2021, we brought on a variant sequencing assay utilizing our next-generation sequencing platforms, the Ion Torrent GeneStudio S5 Prime System, and then in April 2021, we received a contract from the CDC (Centers for Disease Control and Prevention) to perform sequencing on all positive samples.
We’ve been active in the COVID-19 pandemic from a laboratory’s perspective, performing PCR testing, variant sequencing, antigen testing, and antibody testing.
AF: We've been involved very heavily from the beginning of the outbreak primarily in detection assays for determining who has the virus or not, identifying the virus itself, the strains, and conducting epidemiological surveillance, as well as point-of-care testing. Our pharmaceutical manufacturing and bioproduction businesses are heavily involved in the production of vaccines, as well as some of the therapies for SARS-CoV-2.
SS: How has the COVID-19 pandemic increased the need for NGS for virus tracking and surveillance?
JA: The COVID-19 pandemic has highlighted the importance of the NGS technology and generated further investment into developing next-generation sequencing. Innovators like Thermo Fisher Scientific and others have been able to get the assay costs down, where you can test on a wide scale. I think it's extremely important, as we have seen over the past 20 months, that the virus itself has continued to mutate and create variations, which can have different effects on people. So, we need to keep track of when those different variants arise, and being able to do that immediately, in real time, is going to be extremely important for the future of public health.
AF: Most governments and public health agencies around the world sequence a percentage of all the positive tests. What we need to do is identify the genome sequence, because we know that new variants are rising all the time, and Omicron is a classic example of why you need next-generation sequencing. The TaqPath assays have some ability to detect novel variants, and in the case of Omicron, one of the two strains could be identified, because it caused an S-gene dropout. It turned out there's a second version of that strain that doesn't cause the S-gene dropout. You need to keep an eye on the whole genome of the virus to see how it's changing. The Ion Torrent SARS-CoV-2 Insight Research Assay that we developed is designed to be incredibly robust with a large number of redundant primers that cover the sequence so that we can maintain coverage of the whole genome and look at an accurate picture of how the virus is evolving.
SS: Why is comprehensive genomic sequencing needed to rapidly detect Omicron and other new variants?
JA: Comprehensive genomic sequencing is needed because the virus itself has different mutations, and we need to be able to identify those mutations and then the potential subsequent symptoms. We need to be able to determine if there is a pattern to how individuals react, how the vaccine performs, and then provide that data across the continuum of healthcare, whether it be to public health, the vaccine manufacturers, the pharmaceutical companies or even the providers themselves. We must have a targeted effort on how to attack and best make sure that this virus doesn't impact more people than it has.
AF: You need to understand the full genome, not just individual mutations, to know how the virus is evolving. You can understand what known variants are present by doing genotyping with real-time PCR. You can also understand some of the novel variants, if you do capillary or electrophoresis-based sequencing, but that still doesn't give you the full picture. You need to cover 99% to 100% of the genome, and that's why you need next generation sequencing. We’ve seen that the virus evolves so quickly, so we need to understand the picture from a public health perspective to take appropriate action based on new mutations coming into the environment, whether that is in your local area or at a national or international level.
SS: Tell us a bit more about the technology being used to bring sequencing to more laboratories and the importance of rapid turnaround times
JA: The footprint of instruments has significantly reduced, allowing for more instrumentation to fit inside a lab and for more labs across the country to be able to include this as part of their test menu. Also, the cost per test has significantly reduced from five to ten years ago, when it was costing thousands of dollars a sample to run tests. I think the improvements to the technology should help expand sequencing across the board. If processes are made more robotic, and there’s more automation included, it should - and will - decrease the turnaround times, which then provides better quality results to the end consumer.
AF: The technology we use is based on what’s called semiconductor sequencing. The fundamental technology that we use is derived from the semiconductor industry, and it’s a small chip that does the detection of the incorporation of nucleotides. The advantage of that technology is it’s inherently rapid, so our sequencing times are only of the order of about two and a half hours for a sequencing process itself. The Ion Torrent Genexus System can make a fully automated workflow with very little hands-on time and can deliver results in as little as 14 hours for a small number of samples, or less than 24 hours for even a fairly substantial number of samples. What that enables you to do is to put those systems in a distributed setting, so closer to where the outbreak or the patients are, and get answers very quickly so public health officials can have real-time insight into the outbreak in their environment.
SS: Apart from COVID-19, how can NGS be used in other applications?
JA: The landscape is infinite for the use of NGS. We can do whole genome sequencing. We can do target sequencing for cancer diagnostics. Really, if there is something that we need, if there's a genome out there that we need to understand, then we can understand it through next-generation sequencing. So, the applications that exist beyond COVID-19 truly are infinite, and it's just a matter of where those needs arise within healthcare or within research.
AF: There are a lot of different applications that NGS is involved in. The primary ones that we are involved in are oncology applications, so we are heavily invested in developing various applications to cover solid tumor therapy selection via the Oncomine Dx Target Test. The Oncomine Dx Target Test is FDA approved in the U.S. and CE-marked in the European Union . With 80% of cancer patients treated in community hospitals, our focus is on making NGS testing accessible for more patients. We introduced the automated Genexus System to help unlock access to the right therapy, right away, for more patients. It is currently available for research use and we are preparing for the new IVDR (In Vitro Diagnostic Medical Device Regulation) legislation in the EU and planning to bring the system through the FDA’s approval process in the U.S.
We have a lot of tests that are used in research and by labs in a validated environment to detect mutations in both solid tumor and hematological cancers, as well as a variety of other cancers as well. We're also involved in a variety of other infectious disease areas, including tuberculosis, and we’re working on HIV and inherited disease testing. If you are unfortunate enough to be a carrier of an inherited disease, we have assays and tools that can detect those mutations and interrogate for the unfortunate case where children are born with inherited diseases.
