Accelerating Early Drug Discovery in Auto-Immune and Inflammatory Disease
How cross-functional collaboration between academia and industry is advancing drug discovery in the ULTRA-DD program
17 May 2018

Dr. Louise Berg is an associate professor at the Karolinska Institute in Stockholm, Sweden, with a passion for drug discovery and development in the field of autoimmune and inflammatory disease. She plays an integral role in the Ultra-DD project, a collaborative programme that brings together experts in industry and academia to validate novel drug targets in diseases of the immune system. Dr. Berg is due to present a fascinating insight into her work at SLAS Europe 2018, in Brussels at the end of June. We spoke to Dr. Berg to grab a sneak peak into her research ahead of the much-awaited symposium.
Q: Can you briefly introduce yourself and your place of work?
I work at the Karolinska Institute in Stockholm, within the unit of rheumatology. For 10 years I have worked as a team leader in research as part of a collaborative effort between academia and the pharmaceutical industry. My background is in biology, more specifically within cellular immunology. During my Ph.D. at Karolinska Institutet, I studied T cell derived cytokines in rheumatoid arthritis. I have also spent 10 years studying human natural killer (NK) cells in autoimmunity diseases and viral infections.
Q: Could you tell us more about your work on Chronic Inflammatory Diseases?
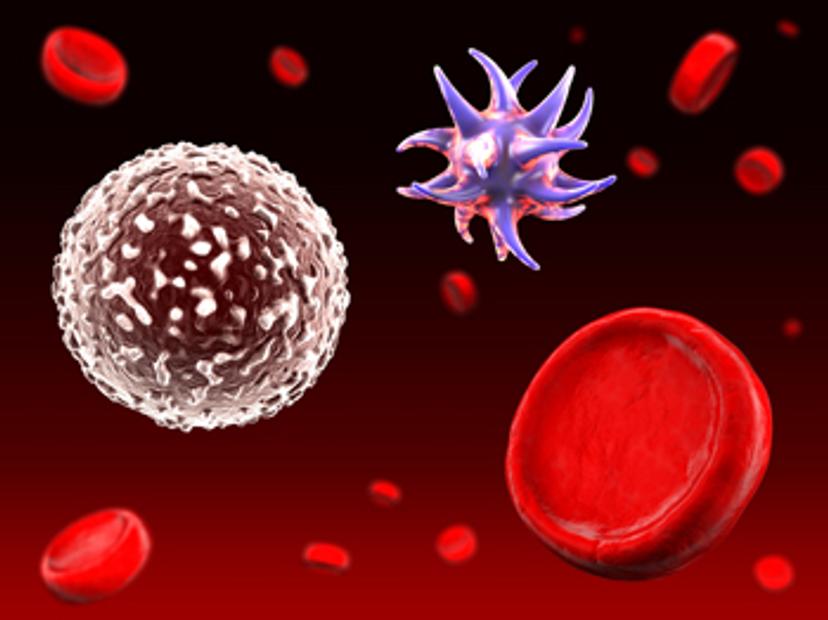
For the past three years, I have worked within a project run by a public private organisation called the Structural Genomics Consortium. The project, ULTRA-DD, is financed by the Innovative Medicines Initiative (IMI) and we have some of the world’s largest pharmaceutical companies as collaborating partners. We aim to be part of early target identification for future drug development in chronic inflammatory diseases, in an open science setting. Within my group, we set up cell assays to screen well characterized and highly specific small molecules. The cells we use come from blood or tissue from patients with chronic inflammatory diseases such as SLE (systemic lupus erythematosus), myositis, systemic sclerosis and inflammatory bowel disease. We believe that by using cells freshly isolated from patient tissues, we can study disease-relevant processes and thus easier identify targets of importance in these diseases.
Q: What exactly is the ULTRA-DD program?
The ULTRA-DD (unrestricted leveraging of targets for research advancement and drug discovery) is run under the Structural Genomics Consortium, with several academic and industrial collaborators. It aims to identify and validate under-explored novel targets in autoimmune and inflammatory diseases. This is done by creating and profiling target-directed chemical and antibody probes in patient-cell derived assays.
My greatest achievement in my work so far has been initiating this programme. This has included recruiting a small team of scientists, equipping a functional laboratory, initiating collaborations with clinics from the hospital and ensuring the recruitment of patients.
Click here to visit our Drug Discovery Community >>
Q: In terms of recruiting patients, how many samples are used in your screening studies and where are they derived from?
At present, for each screening, we use around 10 patients, and a similar number of healthy donors. We work mostly with blood cells, but also with primary skin fibroblasts and biopsies from the large intestine.
Q: Which experimental platforms and technologies do you use to identify and validate these highly specific small molecules?
Since we focus on identifying novel targets for drug discovery in inflammatory diseases, many of our experimental platforms are specific to cellular immunology applications. We use ELISA to detect the secretion of IgG from stimulated PBMC (peripheral blood mononuclear cells) as well as the secretion of pro-fibrotic collagen and cytokines from skin fibroblasts. We also work with a live-cell imaging system, where we analyze the migration and proliferation of skin fibroblasts, the chemokine-induced migration of blood neutrophils, and NETosis of blood neutrophils, as well as much more. NETosis is a relatively recent cell death like observation that is associated with the externalization of chromatin and proteases from webs of neutrophils in neutrophil extracellular traps (NETs).
In an explant set-up, we study spontaneous cytokine secretion from biopsies from the intestinal wall. These biopsies are also used to study the effects of inhibitory probes on the transcriptome and to grow colon-derived organoids for semi-high throughput screening of compounds.
Q: Can you tell us about any exciting results emerging from the project so far and what direction your research might take over the next few years?
We are presently validating our first targets in an assay using PBMC from patients with SLE, myositis and healthy donors. We have found inhibitory effects on cytokine-induced B cell maturation and IgG secretion using a few of the probes tested. The initial validation procedure includes titrations of these probes, as well as negative control compounds with a similar structure, but without inhibitory effects on the target. We are now also using siRNA experiments on primary PBMC for further validation of on-target effects.
I hope that in the future drug development will be much faster than it has been over the past few decades. Working in ‘open science’ should facilitate this, in a collaboration between academia and pharmaceutical companies for early target identification.
Catch Dr. Berg's presentation at SLAS Europe 2018 in the Emerging Investigative Biology session at 10:30am on Thursday 28th June
Visit SelectScience booth #414 at SLAS Europe, June 27-29, to meet the team and pick up a free gift.
