From horses to humans: Elucidating how bones heal after a fracture
In vitro studies reveal the underlying biology of bone repair to inform translational medicine
18 Dec 2020

Musculoskeletal conditions such as arthritis, osteosclerosis, and bone fractures not only limit mobility and diminish the quality of life in humans but also have serious consequences for horses. In this article, we speak with Dr. Matthew Stewart, Professor of Equine Surgery at the Veterinary College of the University of Illinois, about his research studying the pathophysiology of bone and joint disorders.
“My enduring clinical interest is in the musculoskeletal diseases of horses,” says Stewart, a trained veterinarian whose current research projects have focused on musculoskeletal cell lineages: chondrocytes, bone cells, tendon cells, and periosteal cells. “By understanding the underlying biology of bones, we can apply it towards a clinical or translational benefit in horses and in humans.”
One key project in the Stewart lab is to understand how bones heal after a fracture. This work requires the team to examine the periosteal cells, present on the outside of bones, that are responsible for bone thickening during skeletal development and in response to physical activity. Appropriate physiological conditions can activate these periosteal cells and initiate bone formation. The study of these cells provides insight into bone fracture healing and offers the potential to exploit these mechanisms to treat complex bone injuries. “When periosteal cells repair a fracture, they don't initially generate bone, they generate cartilage,” says Stewart. “Once the fracture has been stabilized sufficiently, that cartilage is converted to bone. So, one of our key questions is how do these periosteal cells restore their ability to generate cartilage and bone after being largely quiescent?”
Another project in the lab challenges a long-held myth about the negative impact of inflammatory cytokines on joint health by investigating the response of articular chondrocytes to transient cytokine exposure. “The general notion is that all inflammatory cytokines are bad and all chondrogenic growth factors are good,” notes Stewart. “What we’re seeing is that there’s an anabolic effect – a rebound of sorts – where the cells upregulate their own growth factors following transient exposure to inflammatory cytokines and make more matrix.” To extrapolate from this in vitro context, the cells respond by making more tissue.These in vitro experiments involve extensive culturing of the articular chondrocytes. “They're very finicky cells,” notes Stewart. “They need serum-free or extremely low serum media and ascorbic acid. But most importantly, they need to maintain a three-dimensional context. If they’re attached to a plastic surface like normal cell culture procedures, they lose their phenotype.”
After testing multiple workarounds, such as pellet cultures or coating agar on plates to try growing chondrocytes in the early 1990s, the Stewart lab finally established its protocols using the Costar® flat bottom ultra-low attachment plates by Corning Life Sciences, and have kept up that method for over 25 years. “These plates have been fantastic,” says Stewart. “We just load the cells in there, they sink to the bottom and eventually, they start binding to one another. Within about a week, we get large, robust constructs that can be pulled out with a pair of tweezers. In terms of achieving a stable chondrocytic phenotype, this cell culture model is unquestionably the best. The cells show a very stable expression of collagen-II and aggrecan at about the same levels as seen in vivo.” This cell culture method developed in the Steward lab was later published in the early 2000s.
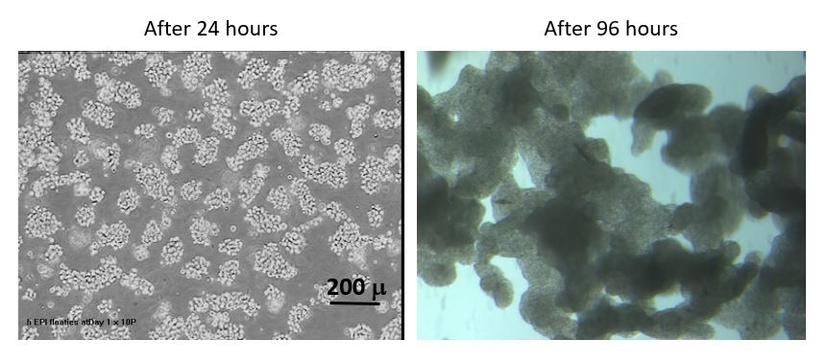
Since then, articular chondrocytes grown using this protocol on the Costar® plates have been used for numerous studies. Stewart notes that one of the benefits of using the low-attachment plates is the selectivity of what cells will ultimately survive under the specified conditions and this is often used as a method to filter out unwanted cells in the mix. “The process with which we isolate chondrocytes can result in a lot of debris, particularly with isolates from murine sources. The good thing about using these non-adherent plates is that the only cells that will ultimately survive are chondrocytes,” explains Stewart. “The first media change removes the debris and gets rid of contaminating cells. What you're left with is a pure chondrocyte cell population.” Cell growth under non-adherent conditions of the Costar® plates also works as a screening assay for certain primary cell types.
Having used these plates for over two decades for multiple research projects, along with other cell culture consumables from Corning Life Sciences, the team appreciates the consistent reliability offered by these products that eliminate variables associated with cell culture methods. “I haven't had to call the technical staff to fix problems because there haven't been any,” comments Stewart.
The outcome of in vitro projects in the Stewart lab is to have a translatable intervention that can be tested in vivo. “For our periosteal bone formation project, our next step would be to move into an in vivo model,” says Stewart. “Currently, fracture repairs are treated with the FDA-approved BMP2, which has increased the cost of orthopedic procedures and generated unforeseen complications, such as excessive bone formation.” Discovering more effective mechanisms for bone repair can make significant contributions towards better treatment options for bone fractures and other musculoskeletal conditions for both veterinary and human health.
Find out more:

