Innovative cell technology enabling new discoveries for B-cell leukemia treatment
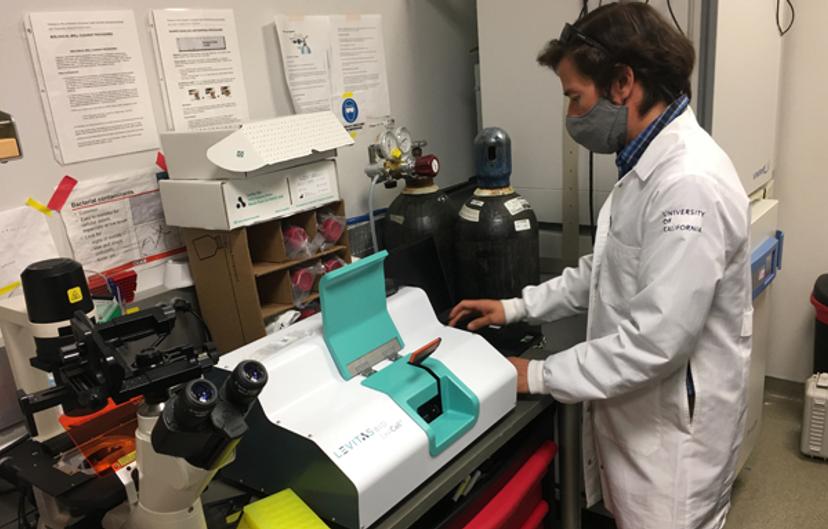
Dr. Ernesto Diaz-Flores, University of California, discusses his work to identify effective therapies for B-cell leukemia, and the cell enrichment platform transforming his research
28 Feb 2022

Hypodiploid B-cell acute lymphoblastic leukemia (ALL) is a childhood leukemia known to be highly resistant to treatments. Understanding the mechanisms mediating this disease is essential in the discovery of new, effective therapies. Research in this field often involves working with limited patient samples, and researchers strive to maximize analyses on these cells.
In this SelectScience interview, Ernesto Diaz-Flores, assistant professor at the University of California, San Francisco, discusses his translational research in B-cell leukemias, from elucidating molecular mechanisms to target discovery through to clinical trials. He also highlights the latest technology streamlining cell-based experiments.
Investigating mechanisms of resistance in B-cell leukemia
Work in the Diaz-Flores lab is focused on hypodiploid B-cell ALL, a subtype of leukemia characterized by loss of whole chromosomes, which is currently difficult to treat. “For some reason, these patients are very refractory to any treatment,” explains Diaz-Flores. Consequently, there is a need to identify new effective therapeutics against this disease.
This journey starts with the analysis of the molecular mechanisms associated with the mutations present in this patient group. “We do what's called transcriptomic analysis, RNA-based analysis, and what we see is how the genes are altered in their expression,” Diaz-Flores, shares. “Then we compare these samples with healthy patients to see what pathways, proteins or genes go up and which go down.” This information is then classified based on signaling pathways. Any promising therapeutic targets can then be identified, and compound screening can be performed to find drugs that induce cell death specifically to the leukemia cells. From here, work ventures into preclinical and eventually clinical trials.
Working with small cell numbers
One of the main challenges Diaz-Flores faces lies with patient samples. “Let's say you get samples from 10 patients. From those patients, you receive the diagnosis and relapse sample. That's it,” shares Diaz-Flores. These two samples need to undergo multiple analyses, from genomic sequencing to single-cell RNA-seq, and to drug screens or to engraftment in patient-derived xenograft mice, all of which require viable cells. Subsequently, the available sample size and quality places a limit on the analyses that can be performed.
Cell viability in patient samples can be impacted by processing and storage conditions at hospital sites. While a sample may start out with 10 to 30 million cells, some of these will die when thawed, during cell culture, and during drug screens. And, when performing experiments with multiple steps, such as CRISPR screens, cells may die at each step. The ability to purify viable cells for further analyses is therefore a great advantage for maximizing the use of patient samples.
New technology for cell enrichment
“We have always been very open to innovation, whether that is new technologies, new approaches or new reagents. Anything that is going to make our experiments easier or faster, or give higher yield or higher purity,” says Diaz-Flores. When LevitasBio approached him about a new technology that could purify viable cells in an easy and gentle way, Diaz-Flores immediately saw the benefits.
The LeviCell system offers users a simplified workflow for label-free cell enrichment and purification. Magnetic levitation is used to precisely separate cells based on their intrinsic properties, including density and magnetic susceptibility. The technology enables users to collect high yields of live cells, even with low input cell numbers – something which has benefitted numerous areas of Diaz-Flores’ work.
His group was a beta tester and evaluated the platform on the separation and collection of live cells from dead cells, in preparation for use in downstream applications. They found the LeviCell system to be an extremely powerful approach in ensuring highly viable cells.
When working with patient samples, high viability is particularly important. To optimize success, viable cells should be purified before experiments. Primary cells do not grow well in culture, so the group used the LeviCell system to select live primary cells after thawing or after short-term cultures to minimize the effect of dead cells to ensure their viability is not diminished for downstream experiments.
The biggest benefits of LeviCell technology for the lab have been found in CRISPR screening. “Nucleofection – the electrical shock used to put the CRISPR construct inside the cells – kills a lot of cells,” explains Diaz-Flores. This is where the LeviCell system is helping to ensure sample quality. “You're able to use the LeviCell immediately and purify your live cells,” Diaz-Flores begins. “Then, the cells can get the CRISPR overnight or over 24, 48, 72 hours without those dead cells.” The system has also helped to improve lentiviral transduction workflows. By purifying highly viable cells, the time required for recovery growth between steps can be reduced. “We use lentiCRISPR approaches, then 24 hours later we run them through the LeviCell,” shares Diaz-Flores. “In this way, we purify highly viable cells, facilitating that transduced cells start growing right away without presence of dead cells in the culture, which would normally impact negatively the CRISPR process, making it lengthier. So, by incorporating this technology we have significantly shortened our timeline.”
Improving CRISPR results
Where CRISPR is concerned, the LeviCell system is already making an important impact on results that would not have been possible using traditional cell separation methods. Previous research by Diaz-Flores identified that BCL-2 is highly elevated and essential in the survival of hypodiploid leukemias. Following successful preclinical results, Diaz-Flores and colleagues began a preclinical trial for the use of Venetoclax, a BCL-2 inhibitor in mice engrafted with patient samples. While this work found that leukemias are sensitive to Venetoclax, a small number of cells still persisted. When treatment was stopped, some mice showed relapse, with the leukemia cells returning.
Diaz-Flores’ work used CRISPR against BCL-2 to further investigate additional genes that may also have a role in driving hypodiploid leukemias. Following treatment with Venetoclax, Diaz-Flores and his team could not distinguish a live cell population using traditional FACS sorting. “We would have discarded the cells, but I decided to put them in the LeviCell in case that there were any live cells. And sure enough, we were able to see a small fraction of cells that clearly “levitated” and were therefore viable,” Diaz-Flores enthuses. These cells were validated as completely knocked out BCL-2 and were further analyzed to identify what had enabled them to remain alive. Analysis showed these leukemia cells were found to have an increase in MCL-1, a survival protein that can rescue the effects of BCL-2 deficiency. “Regardless of how many cells die because of a knockout of any particular gene, we can still see if there is any survival,” Diaz-Flores shares. “We would have not been able to identify those cells if it wasn't for the LeviCell.”
In addition to CRISPR screens, the LeviCell system has also been beneficial in drug screens to isolate relapsed drug-resistant subclones that survived treatment so that these cells can be further characterized. “It's allowing us to focus on the surviving cells, the relapsed cells, the hard-to-treat cells and then, from that, keep doing more mechanistic analysis on them,” Diaz-Flores says.
Other applications and overcoming issues with FACS sorting
In addition to CRISPR, Diaz-Flores has found the enrichment of viable cells achieved using the LeviCell system also benefits preclinical experiments, enabling the use of fewer cells, while also ensuring faster, successful engraftment in mice. The system has also been used by the lab to reduce background noise in downstream applications such as single-cell RNA-seq or DNA sequencing, whereby you can be sure the results you see are due to the leukemia effect versus a result of dead cells inducing further cell death.
Diaz-Flores shares that the LeviCell system has also benefitted other groups at University of California, San Francisco – in particular, those who have struggled with FACS-based cell sorting, for example because cells are too big, as is the case with Drosophila cells. Compared to FACS sorting, the LeviCell system is very gentle. “It doesn't have the shear forces that a FACS sorter does. So, because of that, there is no possibility of inducing some cell death, which can happen with a FACS sorter,” says Diaz-Flores. The LeviCell system is also very fast. “When we are sorting a million cells in the FACS sorter, it might take us an hour, or even longer, depending on the purity of the cells. With the LeviCell, you let them equilibrate for 5 to 20 minutes, depending on how good of a separation you want. And then, when ready, you start the separation process that happens in five minutes, regardless of the number of cells,” Diaz-Flores explains.
A third advantage is that no cells are lost during the enrichment process. The LeviCell system can separate your sample into fractions. “You decide how stringent you want those fractions to be - very close to the live cells and that way you have a pure, viable population, or less stringent if you want more yield,” explains Diaz-Flores. This is particularly useful when you have a small number of cells and do not want to risk sample loss – you have the option to just separate the cells and keep both fractions, rather than just purifying one fraction and losing what remains in the other. Diaz-Flores foresees that LeviCell technology may work for scATAC-seq given that the technology can purify nuclei or for fractionation of organelles, for example mitochondria, or even when working with heterogenous sample types, like heterogeneous tumors, where cells may levitate differently based on density and size
Future research
In the future, Diaz-Flores hopes to culture B-cell leukemia primary cells in vitro. “This has already been achieved with, AML and T-cell leukemia, but not with B-cell leukemia,” Diaz-Flores explains. By identifying culture conditions, in combination with the LeviCell system, he hopes to be able to isolate and grow clones from primary patient samples. This will have a significant impact in the search for treatment of relapsed leukemias – including understanding the mechanisms that lead to a relapse, understanding what makes these cells refractory to treatment, and the development of novel therapeutics that can move quickly into clinical trials.
Find out more about the LeviCell system >>
Related article: Single-cell genomics at the Memorial Sloan Kettering Cancer Center: Developing innovative methods

