Novel multianalyte assay has potential to transform cancer research and treatment
The use of protein biomarkers in oncology is growing rapidly and offers real hope to patients with hard-to-treat cancers
2 Apr 2025
Identifying protein biomarkers is an important step in creating precision medicines for solid tumors, tracking patients’ response to treatment, and monitoring disease progression.
Multianalyte testing of liquid biopsies
Carrying out tissue biopsies is time-consuming for healthcare professionals, and uncomfortable and inconvenient for patients who rarely agree to more than one biopsy. Blood samples – or liquid biopsies – can be taken more often than tissue biopsies and mean that clinicians and pharmaceutical companies can gain a real-time understanding of disease and the dynamics of treatment response.
Researchers want to measure biomarker expression on enumerated circulating tumor cells (CTCs), large extracellular vesicles (lgEVs) and other cell types to discover actionable drug targets. Genomic data from circulating tumor DNA (ctDNA) provides information on the major driver mutations in the tumor, while DNA from individual CTCs gives an insight into treatment resistant clones that may otherwise go undetected from global ctDNA analyses.
Healthcare professionals want to use immunophenotyping to see whether the patient’s immune system is responding to a particular treatment and how it changes according to dose and treatment duration. The presence of rare types of white blood cells, such as persisting CAR-T cells, can also be important indicators of response. RareCyte has integrated its highly multiplexed analysis capabilities in liquid and tissue biopsy to provide these individual snapshots of phenotypic, genotypic, and immunologic data. Each is informative on its own, but combining them together in a multianalyte test and single report makes their utility even greater in the laboratory and clinic.
The power of robust assay development

Jon Ladd, Senior Scientist at RareCyte
Jon Ladd is the technical lead on assay development projects for liquid biopsy and Orion spatial biology services at RareCyte, and his current work involves developing biomarker assays that could change the treatment of prostate cancer and other tumors.
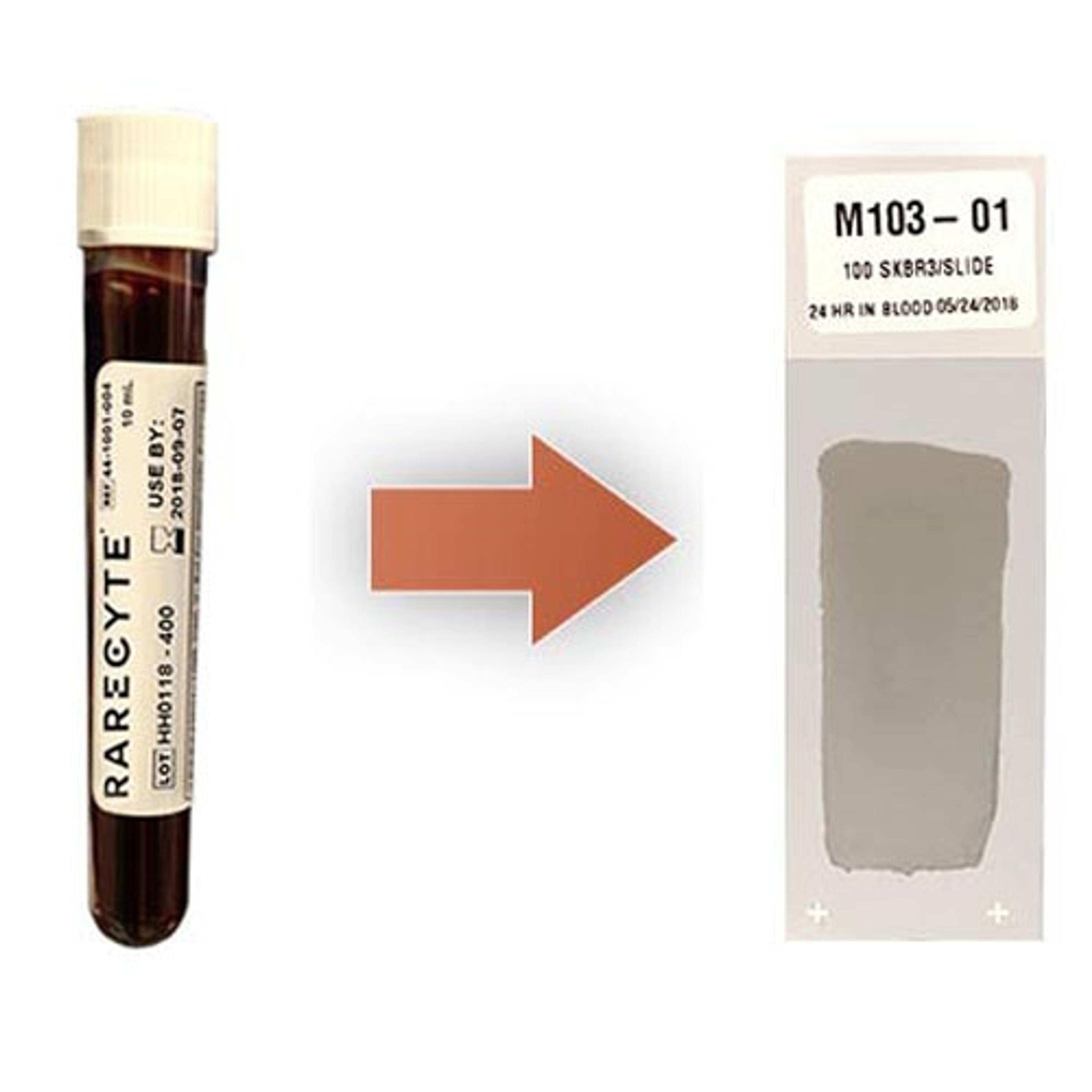
Assay development begins with the collection of a 7.5 mL liquid biopsy (blood) sample in a sterile RareCyte blood collection tube (BCT). The BCT stabilizes and preserves nucleated cells in whole blood for at least seven days prior to processing. The sample is processed using the AccuCyte® sample preparation system, which separates the nucleated cells (buffy coat) from plasma and red blood cells in a density-based, no-wash, no-lysis process. The plasma is separated and stored at –80°C and the buffy coat transferred as a monolayer onto slides with minimal target cell loss. The resulting slides can be stored stably at -20°C for at least three years.
Circulating tumor DNA can be extracted from the stored plasma and sequenced with commercially available NGS panels targeting somatic mutations across common oncogenes and tumor suppressor genes. Buffy coat slides are stained with a custom biomarker assay to measure biomarker expression on CTCs and lgEVs, and to create an immunoprofile of the patient’s peripheral blood. The system also allows enumerated CTCs to be picked from the slide surface and sequenced along with ctDNA.
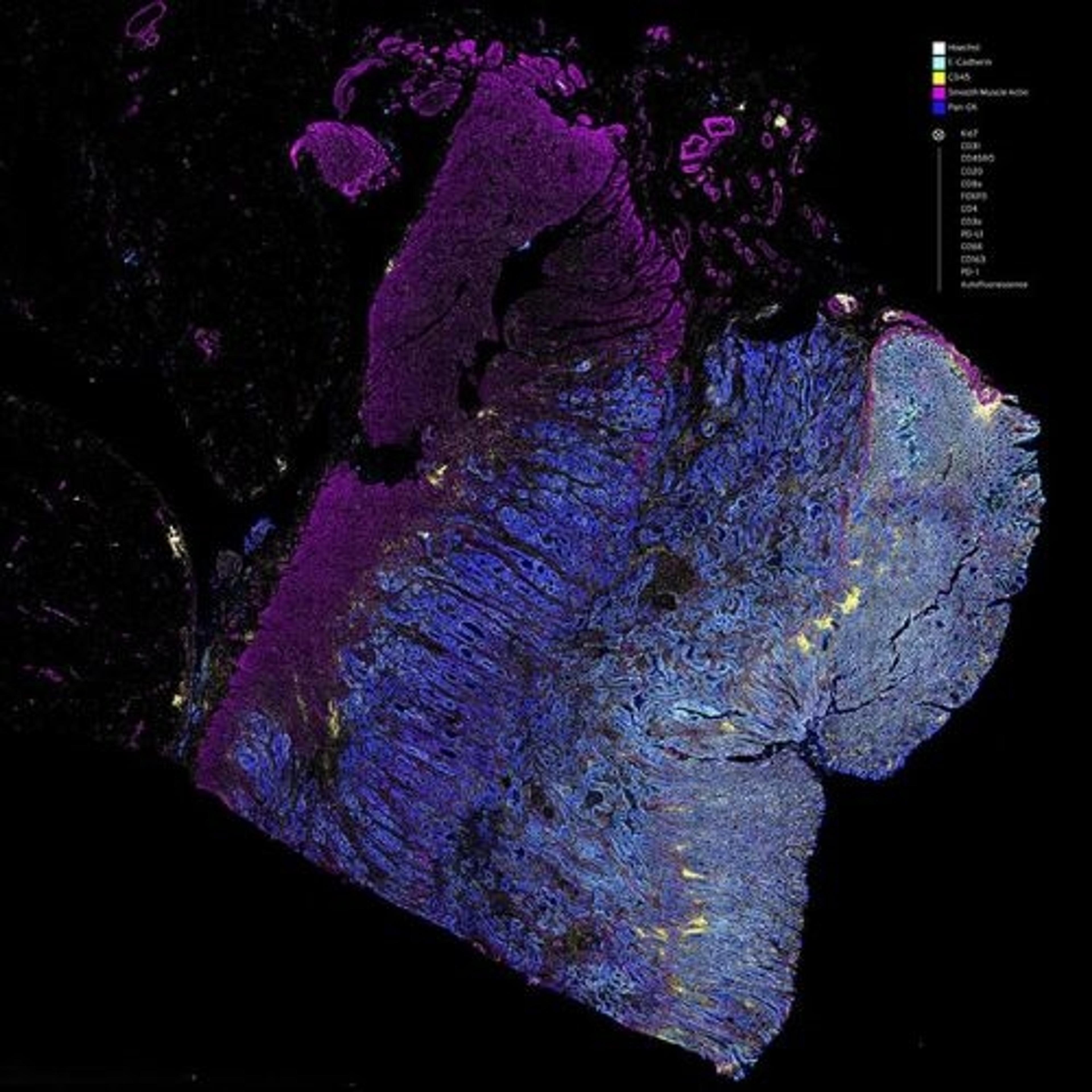
“The Orion™ multiplex immunofluorescence imaging setup allows us to do whole slide staining and scanning following sample preparation. We can carry out fast and flexible panel design with single-round staining and scanning for high-throughput analysis of samples with up to 18 different biomarkers,” says Ladd. “Using this approach, a multitude of information can be collected from a single, 7.5 mL blood sample. Because all sample processing and testing is performed in a single laboratory, clinical trial logistics are dramatically streamlined, and errors with sample handling, shipping, and reporting are significantly reduced. This means that we can create assays quickly, efficiently, and cost-effectively.”

The Orion™ Platform delivers spatial biology and cellular phenotyping at a speed and resolution needed for translation from research to the clinic.
To develop the multianalyte testing approach, the flexibility of the Orion system is leveraged to construct custom 18-plex biomarker panels to quantitatively profile a wide range of immune cells of interest. Markers to differentiate WBCs broadly into T-cells, B-cells, macrophages, etc. could be supplemented with more granular subtyping of T-cells into Cytotoxic (CD8) and Helper (CD4) cells and macrophages into M1 and M2 phenotypes. T-cell activation markers, such as CD45RO, Granzyme B, etc., and proliferation markers, such as Ki-67, can provide a more granular analysis of these immune phenotypes to investigate how the patient immune system responds to treatment. These custom panels allow for unprecedented sensitivity, flexibility and depth in characterizing the immune response to disease.
Creating an assay for prostate cancer
Ladd’s initial goal was to create a dual biomarker assay for prostate cancer, focusing on ARv7 and PSMA, both prostate cancer protein biomarkers expressed on CTCs. ARv7 is a splice variant of the androgen receptor marking resistance to androgen receptor axis-targeted treatments. Its presence corresponds with poor responses to these therapies. PSMA (prostate-specific membrane antigen) is highly expressed on the membrane of prostate cancer cells, and the first PSMA-targeted therapeutic and associated diagnostic has reached the market (Novartis’ Pluvicto/Locametz).
“We began development of each biomarker by screening multiple antibody clones on control cell lines,” says Ladd. “This determined which clone shows the largest separation of biomarker expression between positive and negative control cells. We also looked to see which clones are more compatible with our fixation and antigen retrieval steps than others, which meant that we could get higher specific binding to positive cell lines or have better staining on a particular autostainer.”
Ladd and his team titrated the selected clone to obtain an optimal concentration that maximizes signal to background, and then ran the final assay across multiple slides and multiple stainer runs to ensure a high reproducibility and repeatability of the assay.
Patients who respond to a particular therapy will see a decrease in the number of CTCs in subsequent blood samples. As the assays will be used to observe any response-related decrease during longitudinal clinical studies, an important step of their development is to understand the feasibility of using them in a clinical or research setting. Ladd and his team tested theARv7/PSMA assay in a range of clinical samples taken at partner sites.
“We processed each sample in-house and stained with the optimized assay to count the number of CTCs in each sample and measure their levels of biomarker expression,” says Ladd.
In model cell lines, the ARv7/PSMA assay demonstrated high accuracy, sensitivity, and specificity for ARv7 and PSMA. In clinical samples, the assay was able to detect and classify biomarker positivity on CTCs from late-stage prostate cancer.
“While ARv7 and PSMA are of specific interest to prostate cancer, we can develop assays to measure expression of any protein biomarker of interest on CTCs, lgEVs and other cell types,” says Ladd. “The assays could also be developed into companion diagnostics [CDx] for specific therapies.”
The future of multianalyte testing
By integrating the quantitation of drug target biomarkers and comprehensive immune profiling, multianalyte testing can provide a wealth of specific information that can characterize an individual’s disease. Multianalyte testing allows healthcare professionals to make and modify personalized treatment plans in real time. This has the potential to transform patient treatment.
“We are continuing to develop biomarkers in concert with pharmaceutical companies. This will expand testing capabilities to include additional specific drug targets and response indicators, and to cover more tumor types. We are also exploring ways to include single cell RNA analysis which can provide additional insight into tumor cell function at each tested timepoint,” says Ladd. “I’m really excited to see the positive impact that multianalyte testing can have on patient lives.”