Predicting drug responses using pancreatic cancer organoids and multimodal plate imaging: Your questions answered
Watch this on-demand webinar to discover how pancreatic cancer-derived organoids can be used as a predictive tool for personalized medicine
2 Aug 2020

Pancreatic cancer is a deadly malignancy with few treatment models. Monolayer cell culture has failed to predict patient drug responses in the past. In response to this, a patient-derived organoid (PDO) methodology has been developed that enables the generation of models, from both surgically resected material and biopsies, with a success rate of 75-80%. These cultures enable the molecular dissection of treatment responses and resistance.
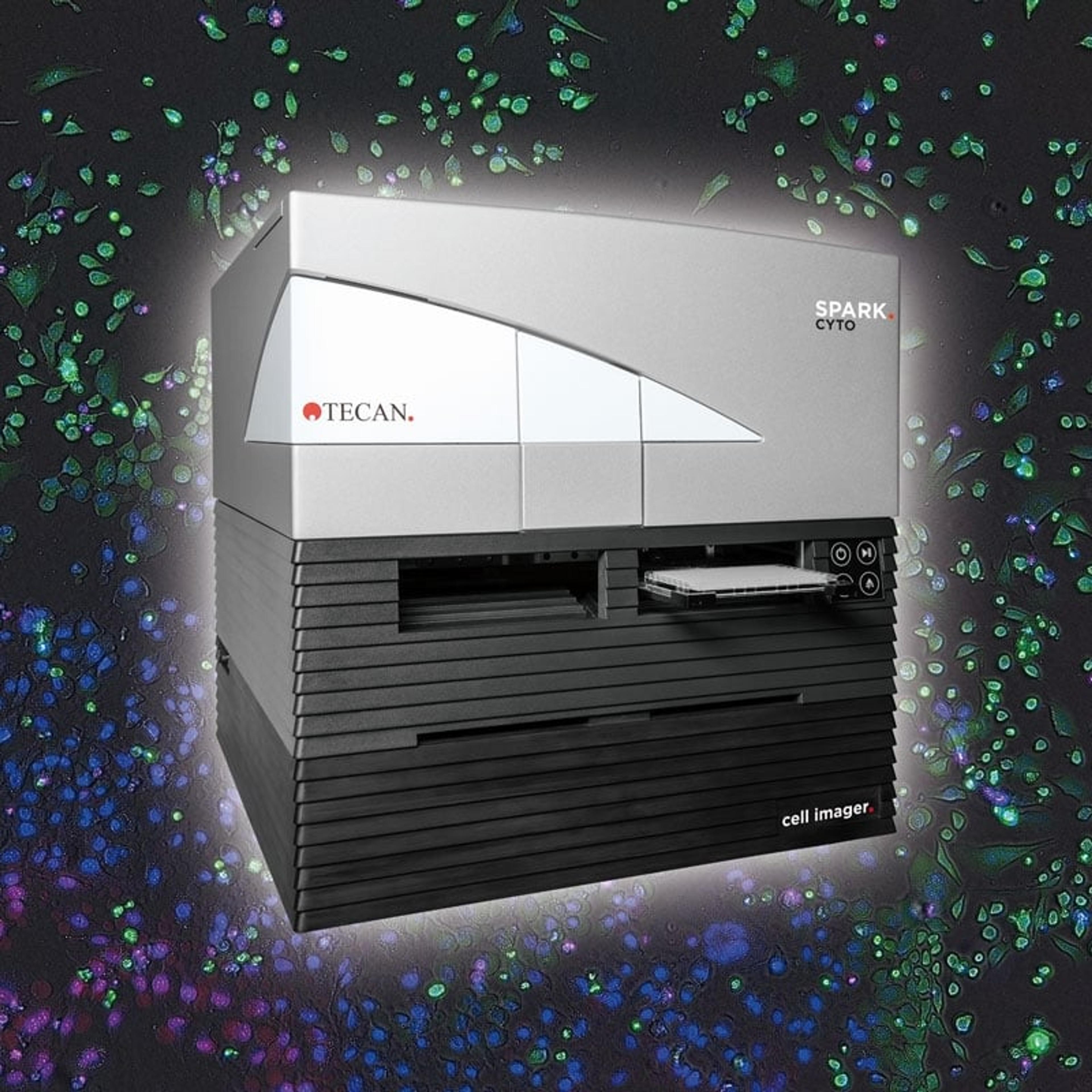
In this on-demand SelectScience® webinar, Dannielle Engle, assistant professor at Salk Institute and Christian Oberdanner, senior application scientist of Tecan Austria, discuss the use of the Tecan Spark® Cyto to evaluate drug responses in PDO models. Given the diversity observed amongst pancreatic cancer patients and the PDO models, they explore how dynamic measurements provide additional flexibility and information for precision medicine approaches.
Read on for highlights from the live Q&A session or register to watch the webinar at any time that suits you.
Watch webinar now
Q: Are the imaging processing algorithms integrated into the Spark® Cyto, or is this something that needs to be done externally?
CO: Imaging processing algorithms are integrated into the Spark® Cyto, and image processing is fully automated, so you do not need to stitch images or create overlays. Images acquired with the Spark Cyto can be automatically processed with our proprietary imaging software package, the Image Analyzer, offering easy data analysis for object segmentation, counting and gating. The new software package also supports multicolor applications so that users can determine which objects emit multiple signals.
Q: Does handling and preparation of patient-derived organoids require a higher biosafety level requirement, or is BSL-1 sufficient?
DE: The risk associated with generating organoid models in cells is the same risk that you have when you are working with serum or plasma, that is bloodborne pathogens. Working with BSL-2 level material is a restriction at your lab. You can access these patient-derived models and after the first passage, there will be no more blood material remaining, so they become much safer to work with. If you remove that first-generation step, you can reduce the biosafety level. This is something that the Human Cancer Models Initiative and the National Cancer Institute (NCI) are doing, creating a repository of patient-derived models.
Q: Did you experience different speeds of organoid formation from the patient tissue? Was this slow, moderate, or fast growth, and how long did you wait to determine successful formation?
DE: We built a model system that recapitulates the diversity that we see in patients. That means that when you have patient tumors that grow slowly in a patient, they are also going to generate a slower organoid model and vice versa. We see a tremendous amount of diversity between the different patient-derived organoid models, some of them grow slowly and it takes a couple of weeks for them to be passaged, whereas some of the models grow much faster and they could be passaged within a week or even faster. When we are generating a new organoid model, we give them a long time to decide whether they are generating organoids. We also have an additional metric where we do not call it a successful organoid generation unless they have been passaged at least five times, meaning that it is a stable model for long-term propagation.
Q: Since you allow reformation of the dissociated organoids, what is the average size? Did you see a gradient, so a drug intensity gradient that was stronger on the edges and weaker in the center of the patient-derived organoids?
DE: When we perform drug testing, we dissociate the organoids down to single cells. The size in which they are going to be at the time that they are exposed to a drug depends on their growth kinetics. That is going to be diverse depending on the organoid line you are working with, so having a single-cell dissociation means that they start at the same point. Some of the organoids are solid, whereas others are more cystic. What we have observed so far is that we do not see a big difference in terms of drug exposure in small-sized organoids. If we were to wait several days instead of 1-2 days, the organoids would have a larger diversity in size, and we might see more gradient effects. With the drugs that we are working with, these chemotherapies do not have a diffusion problem at this small size.
Q: Which method would you recommend using, confluency or ATP assays?
DE: You can use both, and they are not mutually exclusive. Confluency measurements are something that you can do longitudinally, whereas ATP assay is an endpoint assay which involves lysing the cells. With confluency, you can read as many measurements including growth curves and growth kinetics instead of a single data point. I would usually recommend doing as many assays as possible to try to understand whether this reduced viability (CTG) signal is due to apoptosis or it is just the static effects. The more data, the better, especially since confluency measurements do not add to your experiment time or preparation. It just gives you additional information. I would recommend both if possible.
Q: Does the instrument support whole-well imaging for 6- to 48-well plates?
CO: Yes, it does. The unique thing with Spark Cyto is that it supports whole-well imaging for 96-well plates and 384 in one shot. That means one field of view covers the whole well. For the other plate formats, you can have the whole-well view by recording individual images inside the well. Then these individual images will automatically be stitched together to create a whole well view.
Q: Can patient-derived organoids remove the need for clinical trials in the future, especially in the fields of drugs and vaccine development?
DE: The evaluation of patient-derived organoids in clinical trials is still ongoing. I think organoids are something that can be done in conjunction with clinical trials and that clinical trials cannot be replaced. Cell-intrinsic phenotypes do not tell us how drugs are going to behave in the presence of vasculature, circulation, and metabolism by the liver. There are many things to evaluate in a clinical trial so organoids will not be able to completely replace that. However, they can certainly tell you about the mechanism of action, sensitivity, and resistance. I think that they are more designed to better understand and develop individualized patient responses.
Q: Do you get organoids of normal cells in a tumor cell organoid, and if so, how do you get rid of these normal cells?
DE: We have developed organoid conditions that support the growth of both normal and tumor cells. To be more selective for tumor cells, there are a couple of growth factors that normal pancreatic ductal organoids need that tumor organoids do not, so we can remove those from the media when we are isolating the pancreatic cancer organoids. We discovered that it is more selective for the cancer, but normal contamination is something that we test for and we are careful to evaluate that when we generate patient-derived organoid models. We always make sure that the genetics in the organoid match the patient's primary tissue sample to determine what type of KRAS mutation is present. For example, if you have too much normal contamination, you would not see that KRAS mutation. Within just a few passages, we can get pure neuroplastic cultures.
Q: Drug exposure ex vivo is very different from a tumor's exposure to drugs inside the human body. Do you account for drug pharmacokinetics in estimating patient responses and do you think the Area Under the Curve (AUC) can capture such effects?
DE: The pharmacokinetics of estimating a patient response is going to be limited in any ex vivo model since we do not have an intact vasculature and there is no metabolism by the liver. Therefore, we start off with evaluating cell-intrinsic responses. The next step is integrating more complex aspects of the tumor microenvironment, such as inclusion of fibroblasts and macrophages. The final step is transplanting these organoids back into an immunocompromised mouse to evaluate the presence of a desmoplastic reaction in a tumor microenvironment and vasculature. Do we still see efficacy, or is there some resistance mechanism that is stromal-mediated that we have not yet accounted for? When we do these studies, there is a lot of validation that needs to happen to ensure that we are not overestimating treatment response in these model systems. It is something that requires careful consideration in terms of the cell-extrinsic effects that we must incorporate.
Q: Patients are treated with chemotherapy cycles until progression occurs, whereas patient-derived organoids are only treated once. Would mimicking chemotherapy cycles enhance the predictive value of PDO?
DE: Patients do receive iterative cycles of chemotherapy. We could repeat exposure to different drugs and pancreatic organoids to create resistant lines. We are using an accelerated model system, where these organoids are dividing quite rapidly. The timescale is different than what is happening in patients versus what is happening in organoids. However, we can certainly try to evaluate whether durable responses or early transient responses are present in the organoids to try to see if this better predicts patient response.
Q: How do you make sure that physiological conditions are maintained?
DE: Physiological conditions can be a broad statement. If we are talking about temperature, glucose, CO2, and humidity, these are conditions that can be maintained in a tissue culture model. Pancreatic cancer is unique, in that it is hypovascular, and there is limited supply of nutrients and metabolites, that causes the pancreatic cancer to scavenge at a much higher rate than other cancers. Physiological conditions such as vascularization of the tumor are much more difficult to recapitulate in a pancreatic cancer organoid model, but we are trying to add to the complexity by incorporating things like the stromal compartment in co-cultures. We validate this by transplanting these organoids back in vivo and this is usually when we are evaluating different novel drug combinations and gain a clear understanding of the mechanism of action. With the precision medicine pipeline, you cannot wait six to eight months to have in vivo validation to impact patient care because by then the patient would be dead. We are trying to find a balance of what we can model in a timeframe that is relevant for pancreatic cancer patients in a safe manner using drugs that are FDA approved and currently given to patients.
Q: You must use a lot of growth factors to make organoids grow. Is there any possibility of changing the features of a tumor?
DE: When we developed this model system, we used the minimum growth factors required to propagate both normal and tumor organoids with high efficiency. That includes growth factors such as R-spondin, EGF, FGF, gastrin, and these have been shown to be necessary for differentiation and maintenance of the pancreatic identity. Inevitably, these are going to impact biology, and there are a few different metrics to consider. For instance, is this creating artifacts or is this an accurate reflection of human physiology? What we've done is compared a lot of primary samples and tumor organoids, including determining whether the pancreatic cancer subtype is maintained transcriptionally in the presence of different growth factors.
If you have a patient with basal-like pancreas cancer, it generates a basal-like organoid model. If a patient has classical pancreas cancer, it generates a classical organoid model. These are very heterogeneous cancers that are often oligoclonal and so we've done some single-cell sequencing and compared the primary and tumor organoids that way, and we see that the organoids do maintain the oligoclonal representation that's observed in the primary as well as the gene expression patterns. It does seem like we are not creating some sort of artificial signaling programs by using this media system. While you can remove some of these media components transiently, for example, if you are interested in redox metabolism, you can remove the N-acetylcysteine and the EGF. However, these models will stop propagating long term, which requires expansion conditions. If you want to do endpoint analysis and you are worried about certain growth factors or a component, you can take it out for one or two passages for endpoint analysis.
Q: For co-culture systems, are you using cancer-associated fibroblasts and macrophages from the same patient that the organoids are coming from?
DE: When we generate a patient-derived organoid model, we try to isolate and match fibroblasts. We are also going to implement collection of peripheral blood mononuclear cells so that we can isolate the monocytes to derive macrophages. During the optimization period, we are using mouse organoids as well as mouse fibroblasts and bone marrow-derived macrophages to determine the conditions. Ideally, the human organoid co-culture system would use matched components from the microenvironment. We can transform the fibroblasts and we can bank as many PDMCs as possible, but in terms of being able to isolate all these populations from the tumors and keep them propagating indefinitely, that is quite difficult. Inevitably, we will have some patients we can do that for, but not all. We are still determining the success rate of isolation of those two individual components at the same time.
Q: Were you able to grow organoids from patients treated with neoadjuvant chemotherapy? Do you modify the protocol in some way in this case?
DE: The more successful the neoadjuvant therapy, the less likely viable cancer cells are going to be present. Depending on how successful this treatment was, we might have insufficient viable material to generate the organoids. It is always more effective if there is either some period after the chemotherapy or before the neoadjuvant therapy. If you have a diagnostic biopsy, a single pass is enough to generate an organoid model. This way you are not solely relying on material after the neoadjuvant treatment because we have seen tumor specimens from patients that have received neoadjuvant therapy and have no viable cancer cells present.
Q: Do you control the compactness of spheroids when reforming them?
DE: The compactness of the spheroids or the organoids varies from patient to patient. We do not control them, besides the fact that these do go down to a single-cell suspension at the time of plating for drug testing. As they reform, a lot of these organoids will be solid or cystic, depending on the patient's primary tumor morphology and so that is not something that we control for. That is something that is an inherent variable of having an accurate patient-derived tumor organoid model.
Learn more about pancreatic cancer-derived organoids: Watch this webinar on demand >>
SelectScience runs 3-4 webinars a month across various scientific topics, discover more of our upcoming webinars >>