The Importance of Early Diagnosis in Alzheimer’s Disease
There are several promising areas of research that could enable earlier diagnosis of Alzheimer’s disease
11 Jan 2016

Dr James Hendrix, Director of Global Science Initiatives, at the Alzheimer’s Association The Alzheimer’s Association The Alzheimer’s Association's mission is to eliminate Alzheimer’s disease through the advancement of research, to provide and enhance care and support for all affected, and to reduce the risk of dementia through the promotion of brain health.
Research on new strategies for earlier diagnosis is among the most active areas in Alzheimer's science. Funding from the Alzheimer's Association has spurred significant advances and steady progress. Dr James Hendrix, Director of Global Science Initiatives, at the Alzheimer’s Association tells Sonia Nicholas, SelectScience®'s Clinical Editor, about current research studies aimed at diagnosing this ultimately fatal disease.
SN: Dr Hendrix, please could you start by telling us a little bit about Alzheimer’s disease and how many people it affects?
JH: Alzheimer’s disease is a chronic, progressive neurodegenerative disease that affects mainly the older generation, although a rarer, early onset form does also exist. Alzheimer’s disease is characterized by memory loss, difficulties in thinking, loss of visuospatial skills, and problems with language, concentration and problem solving. Alzheimer’s is the sixth leading cause of death in the US.
Over five million Americans are currently living with Alzheimer’s disease and the number of cases is increasing every year. Although we don’t fully understand the reasons for the increase in case numbers, we believe that the aging population is largely to blame. This year, Alzheimer’s and other dementias will cost the US $226 billion. If we don’t find a way to slow or stop the onset of this destructive disease, these costs could rise as high as $1.1 trillion by 2050.
Current diagnostics
SN: What are the current methods of diagnosis?
JH: Alzheimer’s disease is the number one cause of dementia, however not everyone with dementia has Alzheimer’s disease. Having an accurate diagnosis enables the patient to receive the right treatment. This is especially important if the patient has a form of dementia other than Alzheimer’s.
Diagnosis typically involves neuropsychological tests that are carried out by a physician. These include tests for attention span and memory, tests for language and speech skills, and tests for reasoning, planning, and organizing skills. This may be initiated by a family doctor, often after a spouse or child raises concerns about an elderly relative. A battery of tests is performed, including in some cases, an MRI to rule out a brain tumor. The tests performed currently are not able to definitively diagnose Alzheimer’s disease, they are carried out to rule out all other possible causes of the presenting symptoms.

SN: Could you tell us about the research projects that the Association is supporting, with regards to diagnosing Alzheimer’s disease at an earlier stage?
JH: There are several areas of research that we are focused on, some are at a more mature stage of investigation than others. Most of this research is focused on the detection of two proteins, amyloid and tau, that are the hallmarks of the disease. We know amyloid forms insoluble plaques outside neurons while tau forms tangles within neurons. Both plaques and tangles become more common as people progress in Alzheimer’s disease and until recently, these structures could only be detected after death during an autopsy.
Imaging - Neuroimaging is one of the most promising areas of research focused on early detection. Alzheimer patients have large amounts of amyloid in the brain. There are currently three radioactive imaging agents approved for use in the US. These agents allow amyloid protein in the brain to be visualized with a positron emission tomography (PET) brain scan.
Despite being approved for use, amyloid neuroimaging is not currently used in routine clinical practice because its use is not reimbursed by Medicare or Medicaid. However, the Alzheimer’s Association believes that more widespread clinical PET screening could positively affect how patients are treated by their physicians. A project starting early in 2016 known as the IDEAS Study (www.ideas-study.org/), supported by the Alzheimer’s Association with substantial funding from the Centers for Medicare and Medicaid Services, plus support from the three manufacturers and the American College of Radiology, will assess the impact of more than 18,000 PET scans and observe their effect on patient care.
A secondary aim of the IDEAS Study is to explore hospitalization rates. It is a hypothesis of the study that a more accurate diagnosis will reduce hospitalization rates.
In earlier stages of research are the use of tau imaging agents, as well as the use of MRI to look at the hippocampus. It is known that this part of the brain, which is very important for memory, shrinks as Alzheimer’s disease progresses, however both of these areas of interest still need to be fully evaluated and investigated.
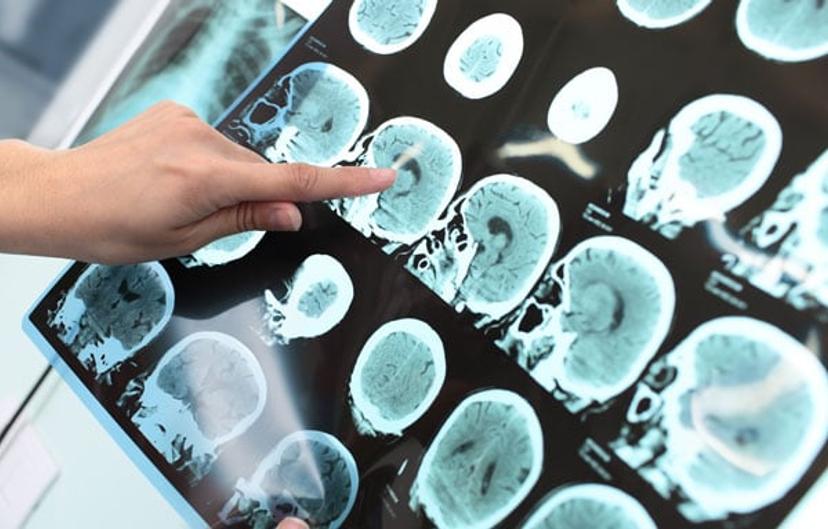
There are currently three approved radioactive imaging agents that allow amyloid protein in the brain to be visualized with a positron emission tomography (PET) brain scan
Fluid biomarkers - Amyloid and tau can be measured in the cerebral spinal fluid (CSF) that circulates in our brains and spinal columns. These biomarkers can give us a sense of how an Alzheimer’s patient is progressing. During disease progression, beta-amyloid levels in the CSF go down, and tau levels increase. However, in order for these biomarkers to be used in clinical practice, there needs to be a way to standardize these test results globally. The Global Consortium for Biomarker Standardization (GBSC), consisting of a panel of scientific experts and diagnostic companies convened by the Alzheimer’s Association, is currently working on this standardization problem.
Blood based biomarkers - The ideal scenario in diagnosing Alzheimer’s disease would be something simple, such as a blood test. There is a lot of work going on around this, for example in the work of Sid O’Bryant at the University of North Texas Health Sciences, however this research is still quite preliminary and the researchers are facing standardization issues.
SN: How could patients benefit from earlier diagnosis of this disease?
JH: It is my firm belief that we don’t have to wait for a diagnostic test to be advocating earlier diagnosis. Even though we don’t yet have a disease modifying therapy, we need to start treating Alzheimer’s patients proactively, rather than reactively.
At some point we have to recognize that a patient with Alzheimer’s is not just undergoing normal cognitive decline; they have a serious, progressive disease. As soon as we know this, we can help the family to prepare for the future. For example, we should be helping them to plan for the day when they have to move their relative into a home, or stop them from being able to drive.
At the moment, far too often we wait for a crisis to happen before step in and intervene. This is the reason why we believe that with screening with amyloid PET imaging will have the secondary effect of reducing hospitalization rates. Take the example of a diabetic patient with undiagnosed Alzheimer’s. The patient forgets to take their medication and ends up in hospital. If we can diagnose Alzheimer’s earlier we can reduce these types of unnecessary hospitalizations.
So even today, without the drugs that we hope to one day have, early diagnosis is absolutely vital.
The idea of being able to prevent disease onset and progression has been made possible because our biomarker research shows that changes occur in our brains as many as 10 years before symptoms appear. Early treatment improves patient outcomes, but it would be even better to prevent the damage before it occurs.
Currently the only drugs we have available are those that help to treat the symptoms associated with Alzheimer’s. We are of course looking for disease modifying drugs as well as additional symptomatic treatments.
SN: When could we expect to see these tests in clinical practice?
JH: I’d love to be able to give you an exact answer to this. But the honest response is that we can’t really know. Amyloid imaging, which is currently available but very expensive, will hopefully be made available to the wider public over the next few years.
CSF biomarkers, the most mature of the biomarker research areas in Alzheimer’s, is looking promising, however it will be several years, at least, before we can hope to see this in clinical practice.
Funding is key
Ultimately, all of these areas need so much more research, and in order for our scientists to be able to carry out this work, we need more funding at the federal level. There are so many good ideas out there that are worthy of further research, but we can’t currently afford to pay for them and this is incredibly frustrating for everyone involved. We need many more opportunities to learn more about this dreadful disease so that we can improve the lives of the patients and their families.
