The tobacco epidemic: The surprising link between macrophages & lung disease
Dr. Patrick Hume shares his mission to investigate how cigarette smoke influences the role of pulmonary macrophages and reveals how his findings could help enhance future therapeutics
10 Apr 2022

Cigarette smoking is one of the leading causes of preventable death worldwide. According to the World Health Organization, tobacco kills more than 8 million people per year, making the global tobacco epidemic one of the biggest public health challenges we face. In this exclusive interview, we speak with Dr. Patrick Hume, pulmonologist and physician-scientist at National Jewish Health, to find out more about his pioneering research investigating the link between lung disease and pulmonary macrophages. Hume and his expert team are on a mission to fight back against this public health crisis by gaining a deeper understanding of the role of macrophages in different locations in the lung, as well as how they dictate how our lungs respond to different injurious stimuli, including the exposure to cigarette smoke. Hume also discusses how Olympus microscope technology helps him reach his research goals and outlines his aims to broaden our understanding of lung disease to save lives.
Smoking and respiratory disease
Macrophages are effector cells of the innate immune system and play a central role in maintaining tissue homeostasis, eliminating damaged cells, and secreting pro-inflammatory and antimicrobial mediators. “We're interested in understanding how the body responds to cigarette smoke, particularly how the airways within the lungs are affected by cigarette smoke,” says Hume. Thanks to medical advances and healthier living, it is now common knowledge that repeated exposure to cigarette smoke can cause direct damage and scarring to the lungs, alveolar spaces, and airways. This damage can eventually result in chronic obstructive pulmonary disease (COPD), emphysema, and many other chronic and incurable conditions.
Hume and his team believe that macrophages are important cells in initiating the immune response that occurs after cigarette smoke exposure and want to better understand the role of macrophages in the lungs. To improve this understanding, Hume’s team is focusing on the role macrophages play at very specific lung locations.
“Some macrophages, including alveolar macrophages found in the alveoli, are present in the airspaces and are responsible for cleaning up particles and promoting lung healing. However, there are also populations of macrophages that exist within the tissue layers of the lungs, such as inside the airway walls and in between the alveolar spaces,” Hume explains. “We're interested in understanding how the location of these particular cells dictates their unique function.”
Interestingly, the number of macrophages present within a smoker’s lungs is significantly higher when compared with a nonsmoker. “We suspect these macrophages are playing an important role in guiding the immune response, and the repeated injury and activation of these macrophages may ultimately result in aberrant wound healing that amplifies the response,” hypothesizes Hume. “I believe too many of these macrophages are a bad thing, but that's still uncertain.” Hume and the team are now trying to understand where these cells are located in the lungs and how their location affects surface expression and genomic transcription.
Helping to end the tobacco epidemic
Smoking has long been linked to the cause and development of many respiratory diseases, yet there remain many unanswered questions and challenges to overcome, particularly for the team at National Jewish Health. “A hurdle of ours is being able to locate good tissue samples and good microscopy techniques to help us better understand the location of the macrophages. What we want to be able to do is tie together microscopy with sequencing and functional assays,” Hume explains. Combining microscopy with sequencing and functional assays will help them understand what roles the macrophages play at different locations, and whether there are multiple macrophage subsets in these locations that are all playing different roles. Hume adds, “Ultimately, the reason we'd like to do this is to understand the impact that macrophages are having on promoting and preventing disease.” If the macrophages are found to limit the response and damage caused by cigarette smoke, the team would want to augment the macrophage activity. However, if they found that the macrophages were injurious and resulted in aberrant wound healing, then they would instead need to limit them. “This can be used to guide future therapeutics and prevent disease occurrence,” he says.
Another key obstacle the team commonly faces is the ability to study macrophages located within many different organs. “For years, researchers have used techniques such as lung digest, where you take a piece of lung from a human or a mouse and expose it to various enzymes to break down the collagen and other connective tissues,” outlines Hume. “Sometimes we’ll also use mechanical digestion to try to remove single cells out of the tissue, which is very useful for performing techniques, such as flow cytometry, to understand the cellular makeup of the lung.” Unfortunately, an issue associated with this process is that the locational information of the cells can be lost within the digest process. “A key challenge in the field has been how do we identify and study these cells, without disrupting their location? That's why we've really focused in on using advanced microscopy techniques and quantitative microscopy techniques, like stereology or morphometry, to understand the location of these cells,” Hume continues. “We’ve also used techniques such as fluorescence microscopy and targeted antibody labeling to understand the expression, transcription, and hopefully function of these cells in their specific locations without disruption.”
New hope for patients
Microscopy has certainly pushed the limits of scientific discovery, enabling us to observe the microscopic world like never before. Despite such success, interpreting microscopic images can be a challenge. “Something that's hindered microscopy-based research techniques for a long time is that anybody can take a close-up image of a specific part of tissue and observe cells, and they could easily make a conclusion about where those cells are and what those cells are doing,” Hume explains. “So, one needs to exercise a lot of caution when interpreting single microscopic images.”
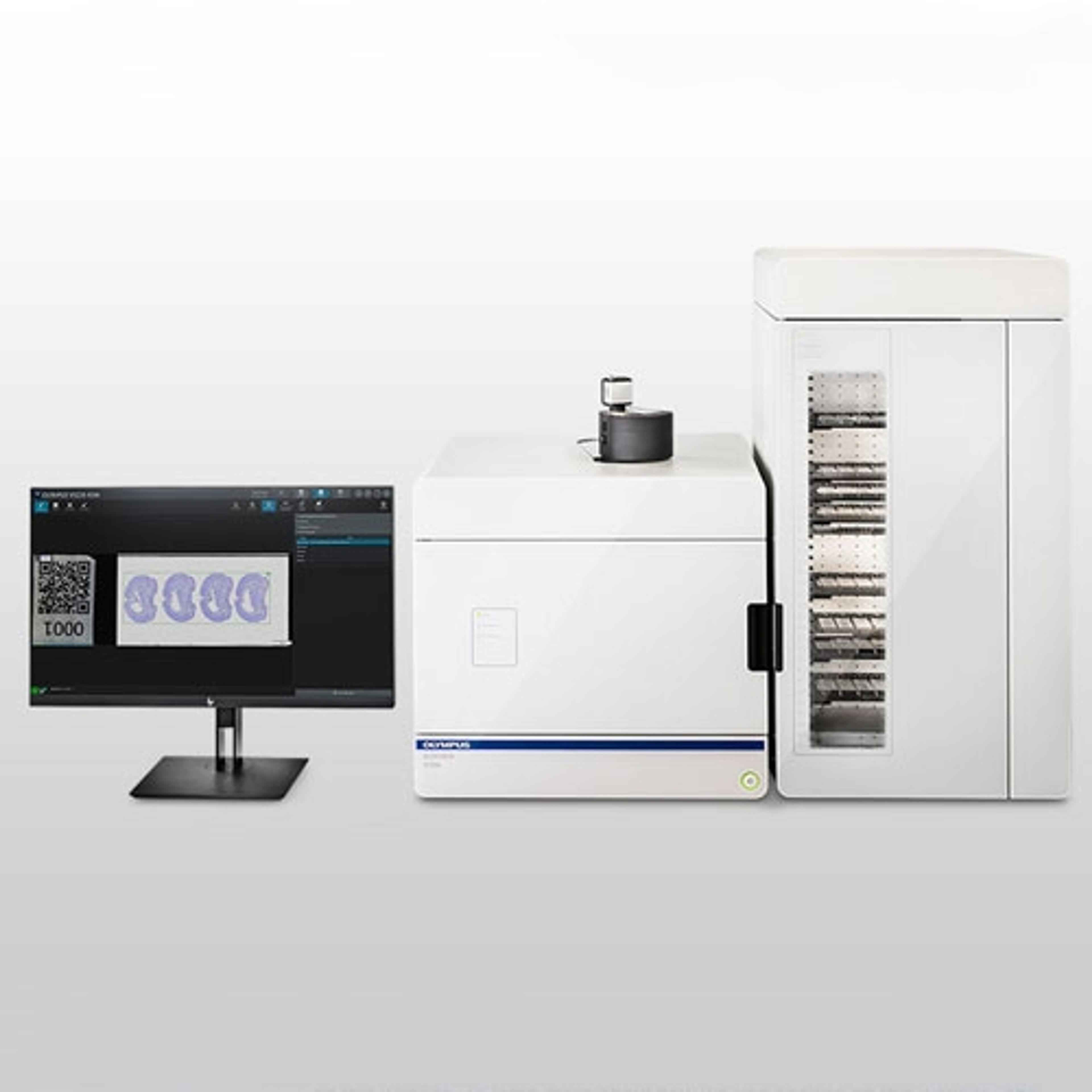
To help overcome these obstacles, Hume is using Olympus’ SLIDEVIEW™ VS200 research slide scanner to capture high-quality virtual slide images. “A key advantage of the VS200 is that it is a very quick, reliable, and high-throughput whole slide scanner,” he shares. “We've come to rely on our ability to perform four to five-channel fluorescent antibody staining, and now we can perform high-throughput imaging of the entire slide to gain a view of what is going on throughout all the different parts of the lung.” This technology is helping Hume and his team understand where the cells are located on a single slide, whether that be around the vessels or the airways. “This microscope is very high throughput, so we now have the ability to scan hundreds of slides at once with a single setup,” explains Hume. “This can really help us gain a bigger picture of the overall structure of the lung.”
The research group pairs this technology with advanced microscopy techniques, including stereology, to help ensure unbiased methods interpret the number and size of the cells. “While stereology alone has been around for some time, a major limitation is that it's very labor-intensive and requires a user to individually take images and quantify them,” he shares. “The key benefit of this technology is ease of use. This technology has been designed in a way that the hardware and the software work very well together, which creates an easy user interface and user experience.” Hume also highlights the quality of the optics and the cameras as another notable benefit. He explains, “We can take very good, clear pictures and have been really impressed with the results that we are receiving.”
Future outlooks
Looking ahead, Hume and his team of expert researchers are on a mission to understand more about the role of pulmonary macrophages and how this research could be employed to help better develop future therapeutics. “We hope to improve human lives and reduce the burden of chronic diseases, including chronic obstructive pulmonary disease and emphysema,” Hume states. “What we really want to do is understand how the cells in the lungs change in response to cigarette smoke exposure and know what role these macrophages are playing.” Hume is hopeful he will soon be able to identify important cell subtypes that could be targeted with future therapies, either to promote beneficial cells or limit the effects of deleterious cells.