Why diagnostic labs are critical for the transition to value-based healthcare
Gillian Hall of Roche Diagnostics shares why diagnostic labs play a critical role in driving a value-based approach to healthcare
2 May 2023

Over the last 15 years, there has been a growing movement towards value-based healthcare as a potential response to many of the challenges facing healthcare systems today. At its core, value-based healthcare is a patient-centered approach to healthcare delivery focused on improving the health outcomes that matter most to patients across the entire cycle of care. But what does value-based healthcare mean for diagnostic labs, and what role can they play in driving this approach?
In this interview, SelectScience® asks Gillian Hall, Roche Healthcare Consulting Global Lead at Roche Diagnostics International, why diagnostic labs are so critical to the transition to value-based healthcare, what barriers need to be overcome, and what healthcare leaders should be looking for in a partner to help them make the shift.
A biomedical scientist at heart, Hall has over 20 years of experience working in healthcare, including 14 years delivering pathology services in the UK NHS. She joined Roche in 2014, building upon her experiences of implementing point-of-care testing in acute and primary care settings, to oversee the entire point-of-care (POC) software product portfolio. Now, in her current role, Hall focuses on delivering services that enable mapping out new ways of working to ensure the full impact of diagnostics on patient care is felt – beyond just providing fast results.
Putting patients first
The concept of value-based healthcare was first introduced in 2006 by Prof. Michael Porter and Prof. Elizabeth Teisberg in their landmark book Redefining HealthCare. “It places patients at the center of healthcare delivery, with a focus on improving the health outcomes that matter most to them across the entire patient journey,” begins Hall. “At the same time, it aims to optimize the use of healthcare resources and the cost to society.”
Value-based healthcare looks to change how care providers define value in healthcare delivery, shifting from measuring volume-based metrics to quantifying positive patient outcomes and the cost to achieve them. “For example, rather than measuring how many hip replacements you're performing, it looks at how many people are feeling better, and getting on with their life the way they want to,” says Hall. “This then feeds into how people are incentivized and rewarded in this system, with an alternative payment approach.” Under value-based healthcare, payment would be based on positive patient outcomes rather than on the number of procedures performed – reflecting the value and not volume.
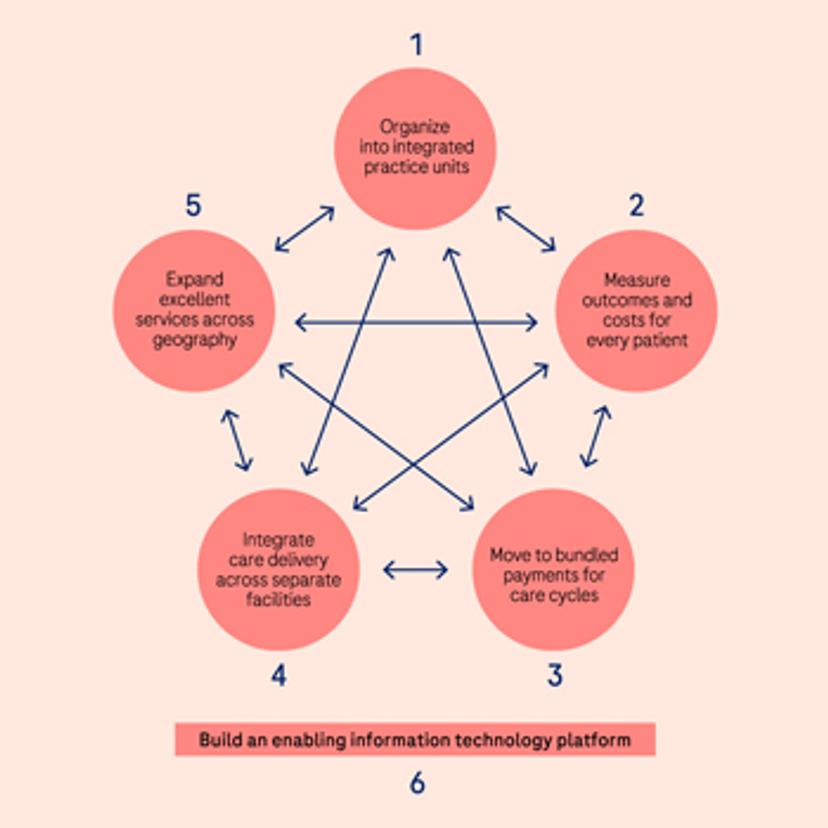
In their original publication, Porter and Teisberg outlined six key enabling components of value-based healthcare. These include structural organization, methods to measure patient outcomes and costs, bundled payments, and the expansion and joining-up of services across the patient journey – all underpinned by ways to manage and share information in the right places and at the right time.
In response to the numerous challenges facing global healthcare systems, such as rising costs, aging populations, and the lack of correlation between expenditure and patient outcomes, the value-based healthcare movement is gaining traction. “Currently, value-based healthcare approaches have mostly been implemented in Europe, but there are examples from across Australia and the U.S. too,” says Hall. “The need for change is very clear and we're certainly seeing an increase in that desire. There is lots of evidence to show that ministries of health are now taking this very seriously, and looking at how they can procure differently, implement services differently, and deliver care in a better and more sustainable way.”
Value-based healthcare: The role of diagnostics
Diagnostics are critical to today’s healthcare system, touching every point of the patient journey, from screening to early detection, treatment management, and monitoring. Under the current paradigm, the ‘value’ of diagnostic tests often revolves around their accuracy, sensitivity, and speed. However, a shift towards value-based healthcare would see tests also evaluated against their ability to positively impact patient outcomes, encompassing factors such as the testing strategy used, the accuracy of decision-making by healthcare providers using the tests, and the wider impact on patient lives.
Hall takes POC testing as an example, noting its potential to enable ‘hospital-at-home setups’ where patients may not need to travel to the hospital as frequently. “Having more accessible testing devices and the ability to either test yourself and stay connected to your physician or have a healthcare professional visit you in your own home, are all great ways to deliver services differently and help improve patient care,” she says. “We often think immediately of direct medical outcomes, which are of course very important, but there are also lifestyle factors, such as disruption to daily life. ‘Can I still take my children to school?’ ‘Can I pick them up, or do I have to go to this appointment?’ – these sorts of outcomes are also important to people. This is where diagnostic tests and the way they are delivered can make a big difference.”
Value-based healthcare also encourages discussion around which tests are adding the most value to patients, and where there is inappropriate testing. “For example, looking at how to get clinical teams out of the habit of always requesting the same test in the same panel, and the consequences of that both in terms of overdiagnosis and underdiagnosis,” Hall adds. “Diagnostic labs are always working with their clinical teams to educate them on which tests are required and when, and that will remain a fundamental part of this shift going forward. The lab needs to have a seat at the table when these discussions are happening to make sure that the journey is fully understood, and the clinical protocols have got the right diagnostic tests correctly mapped out throughout.”
Barriers to implementation of value-based healthcare
Despite several successful examples, its full implementation poses numerous challenges. These include shifting from fee-for-service to value-based healthcare funding models, establishing standardized outcome measures, and developing policies and legal frameworks that support value-based healthcare approaches. “The first challenge is getting internal buy-in, both within labs and the wider hospital, including support from clinical leadership, administrative managers, and other key healthcare professionals,” says Hall. “Having that triangle of stakeholders onboard is crucial to trying something new and changing how diagnostics are currently being delivered.”
Hall notes one of the main reasons value-based healthcare pilots fail is due to a lack of budgetary planning to ensure that the necessary resources are available for successful implementation in the long run. “I've seen lots of pilots that have been very successful, people like them, the patients like them, but there need to be sustainable financial mechanisms in place to make sure the changes can be put into a routine,” she says. “That's often the hardest bit and why it is so important to involve your managerial support early in the process.”
“If you can get the financial modeling cracked, and that is definitely one of the toughest pillars to crack, then in theory, it should flow from there, depending on the staff and skill mix,” she continues. “That's the other challenge for lab leaders: thinking about what skills and staffing they need for the future. If their organization is really shifting in this direction, how do they build their workforce to go on that journey as well? Technology will enable new approaches, but people with the right skills need to be there as well.”
Partnering for success
Given the challenges, working together with external partners can prove to be extremely advantageous for laboratories and healthcare leaders looking to implement new ways of working within a value-based healthcare framework. Hall emphasizes the importance of finding a partner who understands the nuances of the healthcare sector, including the challenges of regulatory compliance, and the importance of combining new technologies and staff effectively to enable new ways of working. “Implementing value-based healthcare requires a significant upfront investment of time and effort, and it's essential to work with a partner who can help you break down the process into manageable steps,” she says. “Change management is a critical aspect of the process, as people are often resistant to change, especially if they have been doing things a certain way for several years.”
Being aware that new solutions may not work for all scenarios is also key. “Patients are not going to be uniform and fit into the mold perfectly, sometimes there'll be exceptions,” she adds, “You need to strike the right balance to make sure the approach works for the majority of patients and that you are also able to accommodate exceptions.”
Where to start
As value-based healthcare approaches continue to gather momentum and new methods of healthcare delivery evolve, it is increasingly important that healthcare leaders stay abreast of the latest industry trends to identify opportunities that enhance the delivery of care while improving overall resource- and cost- efficiencies.
Hall concludes by highlighting some of the resources available to learn more about implementing value-based healthcare, including conferences run by the Consortium for Health Outcome Measurement (ICHOM), The World Economic Forum, and The Value-based Healthcare Center in Europe. “At Roche, we have also run educational seminars for our customers at a country level to look at value-based healthcare as a concept, as well as value-based procurement, which is relevant for healthcare leaders,” she says. “There are many case studies that we can learn from, and we encourage people to think about how they can apply value-based healthcare concepts to their own organizations.”
Roche also has its own dedicated website, Healthcare Transformers, which is a content hub for c-suite and executive leaders in healthcare. The platform offers valuable, insightful, and actionable content from leading experts who share their first-hand experiences, challenges, and solutions on topics surrounding healthcare transformation. “On the topic of value-based healthcare, we currently host a range of pieces including articles, webinars, and eBooks that serve as a rich source of case studies and examples of successful implementations,” says Hall. “It's a great place to start if you're beginning to think about how to apply value-based healthcare, are in the early stages of implementation, or simply want to gain more knowledge on the topic.”
