Hiding in Plain Sight: How to Break Through the Tumor Microenvironment Forcefield
Quantifying and targeting MDSCs, the ‘queen bee of the TME’, could overcome resistance to immunotherapy, Dr. R. J. Tesi tells SelectScience
30 Sept 2018

In recent months, scientists at INmune Bio have taken steps towards breaking through the invisible forcefield of cancer-assisting cells in the tumor microenvironment (TME). Their novel therapeutic strategies have the potential to overcome resistance to immunotherapy and are in early stage clinical trials. In an interview with Dr. R.J. Tesi, Chief Executive Officer and Chief Medical Officer at INmune Bio, we discover why cancers recruit protector cells to the TME and how to poke holes in the immunosuppressive shield protecting the tumor from the immune system and immunotherapy.
The field of immuno-oncology has seen exponential growth in recent years. The natural effectiveness of the immune system to eradicate around 10,000 pre-cancerous cells from our body every day makes it the most established and effective tool available for treating cancer. Yet, the ability of tumors to control, evade and suppress host immune cells is such that one’s innate and adaptive immunosurveillance mechanisms become inert, leaving cancer ‘hiding in plain sight’.
Many of the modern immunotherapies, including checkpoint inhibitors such as anti-PD1/PD-L1 and anti-CTLA4 therapies, aim to ‘re-awaken’ the immune effector cells from this cancer-mediated dormancy, but resistance to treatment in approximately 70% of patients is often caused by the immuno-biologic soup of the tumor microenvironment (TME), whose role is to protect the cancer from the patient’s immune system.
Tell us a bit about yourself and about INmune Bio
My name is Dr. R.J. Tesi, I am the CEO and CMO of INmune Bio. We are a company focused on taking the brakes off the immune system by harnessing innate immunity. The immune system includes natural killer (NK) cells, B and T cells, and immunologically active cells derived from the myeloid lineage, including macrophages and dendritic cells, amongst others. As immunotherapy has become a very high-profile area in cancer therapeutics, we have focused our expertise on solving two of the most important problems in immuno-oncology – resistance to immunotherapy and controlling residual disease. Immunotherapy for cancer is not the only application of our clinical platforms, but it is our current focus.
Our immune system is sat on the sideline eating fish and chips!
Dr. Sami Tuomivaara University of Georgia
Why has immunotherapy become such a hot topic in cancer therapeutics, and how does resistance occur?
In health, the immune system is completely tuned to getting rid of cancer cells; this is called immunosurveillance. When immunosurveillance fails, you can get cancer. Furthermore, you can’t get rid of all of your cancer without a functioning immune system. This means a sound immune system is required to prevent cancer and to treat cancer. Astoundingly, we’ve spent 50 years giving patients chemotherapy, and what is one of the things it does? Kills the immune cells. Have we been killing the human body’s most important system for controlling cancer? We now understand the need to harness this unbeatably-effective tumoricidal process. Harnessing the patient’s immune system to conquer their cancer is the newest frontier in the battle against this deadly disease.
Let’s dive a little deeper into this. The first step in a cancer establishing itself in the patient is to evade the immune surveillance. Once that occurs it often takes 10 years to reach the stage where a cancer has grown big enough to be identified by our current diagnostic modalities. Therefore, our immune system has been ‘convinced’ to let it grow for a decade – it’s been sitting on the side-line watching football and eating fish and chips!
The second step for a tumor to develop further is to establish the tumor microenvironment. The TME is packed full of immune cells, such as myeloid derived suppressor cells (MDSCs), tumor-associated macrophages (TAMs), as well as cancer-associated fibroblasts (CAFs), all of which have been subverted by the cancer to protect the tumor, rather than attack the tumor. These cells work to establish a potent immunosuppressive shield that will blunt the effect of immunotherapies in as many as 70% of patients on checkpoint inhibitor therapy.
How does INmune Bio aim to address resistance in immunotherapy?
With our approach, we’re aiming to poke holes in this powerful immunosuppressive shield so that the cells of the innate immune system, which has all the guns, knives and missiles needed to kill the tumor, are much more effective. That is, the NK cells have the lethal weapons to hurt the cancer, but they can’t get close enough to the tumor to be effective. By eliminating the protector cells in the TME, the immune system can attack the cancer and immunotherapy can become more effective.
The protector cell INmune Bio focuses on is MDSCs — myeloid derived suppressor cells — the “queen bee” of the TME. MDSCs produce immunosuppressive cytokines and recruit other types of cells to join them in the immuno-biologic soup that forms the TME. We suspect patients will respond much better to checkpoint inhibitors such as anti PD-1/PD-L1 and anti-CTLA4 inhibitors in the absence of these cells. This is the premise for our ongoing clinical trial with a novel drug candidate targeting MDSCs. Our studies also aim to evaluate the effectiveness of MDSCs as a biomarker in patients and treatment selection.
Is this a solution for tumors of different origin, location and mutational burden?
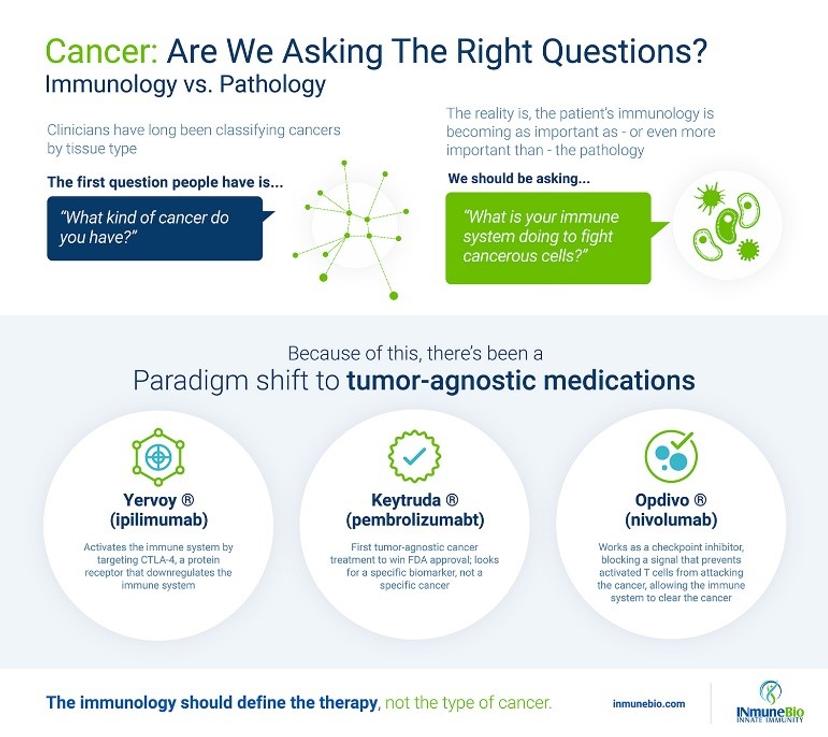
The great thing about our immune targeting approach to cancer is that we don’t discriminate patients based on any of these factors; all I care about is what your immunology is saying. We firmly believe that the immunology defines the therapy, not the pathology (i.e. tumor type and location). Our strategy of using immunologic biomarkers to direct therapy is a novel precision medicine approach that matches the immunotherapy with the patient’s immune dysfunction. Most precision therapies focus on the tumor pathology and ignore the immunology. Personalized is a different kettle of fish! Personalized immunotherapy for cancer, although effective in some patients, can be difficult and time-consuming to make, costly, with results that may be imperfect. Both precision and personalized therapeutic strategies are here to stay; we believe precision medicine is the most practical way forward for patients.
How do you identify the patients that are right for this type of treatment in the lab, and what kind of technologies are you using?
Experts agree that one of the best predictors of resistance to checkpoint inhibitors is the number of MDSCs in blood. Increased MDSCs define a subgroup of patients that have chronic inflammation, where cytokines facilitate proliferation and differentiation of myeloid precursors into MDSCs that migrate to the TME. MDSCs in the TME produce more chronic inflammation and immunosuppression, perpetuating this deadly cycle. We believe about a third of the patients with resistance to CPI have chronic inflammation and elevated MDSCs as a cause of their resistances — that’s about 20% of the CPI patients. If we are right, we can increase the number of patients who respond to CPI from 30% to 50% — how good is that!
We measure MDSCs using 5-color flow cytometers. We also use, as part of our enrolment criteria, C-reactive protein (hs-CRP) as an indicator of chronic inflammation. The specificity of hs-CRP to chronic inflammatory disease has been debated for a long time, but a recent study — following 10,000 cardiovascular patients for five years — has identified hs-CRP as a valid indicator of chronic inflammation. The same study identified that that those with elevated hs-CRP were more at risk of developing cancer. What’s more, hs-CRP can be easily measured in the blood without need for complex technology.
Click here to view multi-channel flow cytometers for use in the clinical laboratory, and here to browse rapid in vitro diagnostic tests for CRP quantification.
How is this technology specific to cancer, if other diseases are characterized by inflammation?
So, acute inflammation is how our immune system responds to wounds and overcome infections — it’s a transient, beneficial process. On the other hand, chronic inflammation is a pathologic process, where the ‘shut-off’ of the acute inflammatory response does not occur and a prolonged, low-level, destructive inflammatory response develops. This occurs in a wide variety of diseases, including neurologic, cardiovascular, gastrointestinal, hepatic and metabolic diseases, and cancer. We prefer the term ‘immune dysregulation’ to define this debilitating immune response because chronic inflammation is not just prolonged acute inflammation, but an immune response that is not beneficial to the host.
Where do you see this work in a few years’ time?
I believe the future is bright. In the future, we believe chronic inflammation will be defined as a disease. Clinicians will recognize that treatment of chronic inflammation is essential to help them recover from the problem that brought them to the doctor. If they don’t treat chronic inflammation as part of the problem, the outcome may be worse. In cancer immunotherapy, we believe this approach has immediate practical applications. The immune response to the cancer has both effector and protector elements. Combination immunotherapy needs to target both, and this will be applicable not just to cancer but also for antibiotics, and other chronic disorders of the immune system.
Do you use flow cytometers in your clinical lab? Write a review today to be entered into a drawing for the chance to win a $400 Amazon Gift card.
