Speeding the transition from bench to bedside with CRISPR/Cas9
Find out how CRISPR/Cas9 KO cell line technology can speed up target identification, validation, and pathway discovery with these insider insights
22 Jul 2020

In this interview, we speak with Dr. Karine Enesa about the benefits of using pre-made CRISPR/Cas9 knockout (KO) cell lines and their potential in the rapid development of gene therapy strategies. Enesa is the head of cell line development at Abcam’s technology department, where her team is responsible for building and delivering a large portfolio of edited cell lines and novel gene-editing platforms.
How has CRISPR technology developed in recent years?
There have been a number of advancements in the CRISPR field that have increased its potential use in both research and the clinic. Recent improvements to CRISPR technology have expanded upon the availability of DNA sequences that can be targeted with this technique. Newly discovered and modified CAS enzymes, for example, xCa9, SaCas9, and NmeCas9, can now recognize more diverse protospacer adjacent motif (PAM) sequences in DNA. There has also been an improvement in the specificity and accuracy of targeting and repairing genomic DNA, which could have huge potential in the future of personalized medicine.
The use of CRISPR/Cas9 has allowed scientists to generate transgenic animal models for research much more rapidly compared to using traditional methods that target embryonic stem cells. We can now directly inject and electroporate guide RNA (gRNA) and Cas9 enzymes into the zygote, which significantly reduces the cost and time associated with producing these animal models.
CRISPR researchers also now have the ability to study gene expression and alter epigenetic states through the use of CRISPR activation and interference (CRISPRa/CRISPRi). These technologies are being used to improve our understanding of transcriptional regulation during development and in diseases such as cancer. For example, CRISPR/Cas9 technology is being used in the clinic to genetically edit patient T cells to express chimeric antigen receptors (CAR-T cells) in vitro for cancer immunotherapy. The resultant CAR-T cells can then be administered to the patient to recognize and kill tumor cells in vivo without the traditional risks of transplant rejection. This immunotherapeutic strategy is showing good potential in clinical trials for the treatment of various blood cancers.
What are the biggest challenges with CRISPR/Cas9 technology?
The use of physiologically relevant human disease models to validate targets and confirm the effect of genes on phenotype is essential to help understand disease states and facilitate effective therapeutic development. The most widely used method of target identification and validation is to knock-down or knock-out the target protein under investigation. However, the CRISPR system still needs refining in terms of efficiency, specificity, and delivery. The production of high-quality KO cell lines and lysates can be technically challenging and time-consuming, amounting to several months of work.
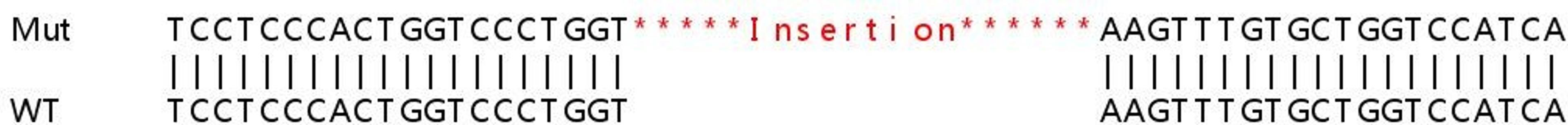
CRISPR can be an arduous process, requiring large amounts of hands-on lab time, and yielding low success rates on average; approximately 40% for KO models and 5% for specific knock-in gene-editing efficiency. Unfortunately, the CRISPR/Cas9 complex can also generate non-specific editing events in unplanned loci, which can lead to off-target mutations. Confidence in your editing relies on designing specific gRNA and being able to accurately predict how the gRNA will bind to sequences in the genome. Various in silico tools exist to predict the binding of gRNA as well as the specificity and efficiency of Cas9 cutting.
There are currently no universal protocols or guidance for CRISPR cell line development across the many cell lines and targets being investigated, so researchers tend to spend time painstakingly optimizing each parameter in the protocol for their specific experiment.
Top CRISPR tips for researchers
- Perform extensive literature research and dig out what has been previously attempted
- Explore multiple strategies, especially for difficult targets, as these experiments might not work straight away
- Identify the skillsets needed and evaluate the possibility of external collaboration or outsourcing of services
How does Abcam’s portfolio hope to help overcome these challenges?
Having a reliable, ready-to-use source of KO cell lines available allows researchers to get on with their target identification, validation, and pathway discovery without first having to establish and validate a suitable KO cell line, saving on cost and effort. Additionally, pre-made CRISPR-Cas9 KO cell lines allow you to quickly and confidently interrogate the relationship between genotype and phenotype.
Abcam cell lines are well characterized and come with Sanger sequence data, western blot validation, a wild-type control, and Abcam’s guarantee of quality. With a wide range of gene KOs in workhorse cell line backgrounds, obtaining your KO cell line is now as easy as buying reagents.
Plus, for more difficult edits or those cell lines that are hard to work with, our gene-editing experts provide full project consultation to remove existing time constraints from your projects, and offer custom services that deliver dependable results in less than half the time taken by the average lab1.
What do you see for CRISPR/Cas9 technology in the future?
Many researchers are currently evaluating the use of CRISPR/Cas9 technology as potential therapies, including gene therapy. There is a huge potential for using and analyzing whole-genome sequencing data and combining this with CRISPR/Cas9-mediated precision editing to identify and correct patient-specific mutations in human stem cells or induced pluripotent stem cells to treat diseases that are untreatable with current approaches.
Hear more from the knockout experts:
- How to achieve research success with knockout models – Dr. Hanna Dreja
- Breakthroughs in guide RNA: Creating successful CRISPR-Cas9 knockouts – Dr. Yongwon Kwon
References
1. Synthego. CRISPR Benchmark Report (2019)